Insurance PPO abbreviation meaning defined here. A preauthorization or prior authorization requirement means the health insurance company requires you to get permission from them for certain types of healthcare services before youre allowed to get that care.
 Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
Polyphenol oxidases a family of enzymes.

Ppo insurance meaning. On the other hand PPO dentists only receive money from the insurance company if services are rendered. The percentage price oscillator PPO is a technical momentum indicator that shows the relationship between two moving averages in percentage terms. A PPO or preferred provider organization gives members flexibility in selecting doctors and other medical practitioners to provide covered services.
PPOs got this name because they have lists of healthcare providers that they prefer you to use. The insurance company contracts with those doctors and hospitals so that they will charge set prices for certain services. Polyp-phenylene oxide a type of plastic Propylene oxide an industrial chemical.
PPO stands for preferred provider organization. Two popular types youll frequently see are HMO and PPO. Get the top PPO abbreviation related to Insurance.
Payment for services received outside the PPO network consists of a percentage split or cost-sharing amount between the member and the carrier. Medicare HMO PPO Medicare also has both PPO and HMO options. PPO health insurance is a flexible and expensive health care option.
Another major perk of PPO plans is that they do not require referrals. A PPO is a health insurance plan that gives you access to a network of preferred health care providers physicians specialists hospitals clinics etc. The PPO means your insurance company will have a network of care providers available to you at your discretion.
PPO health insurance is a group program providing medical services through a network of physicians hospitals clinics and other health care practitioners. Therefore if you already have a doctor that you like you do not need to switch if you prefer not to. PPO insurance also does not require you to choose a Primary Care Physician PCP.
If you get your health care from these preferred providers you pay less. Co-insurance is another disadvantage of PPO plans. HMODMO providers can be expected to perform services for a deeply discounted rate.
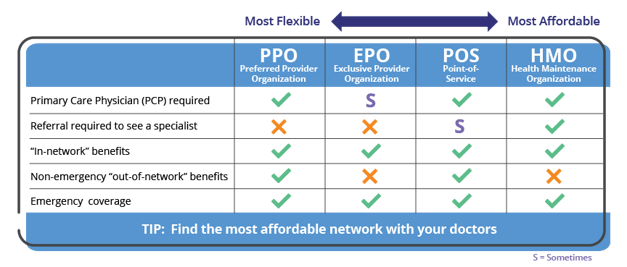
PPO which stands for Preferred Provider Organization is defined as a type of managed care health insurance plan that provides maximum benefits if you visit an in-network physician or provider but still provides some coverage for out-of-network providers. After fulfilling the deductible for out-of-network treatment costs members are still responsible for a portion of any remaining balance. Differences between HMO Health Maintenance Organization and PPO Preferred Provider Organization plans include network size ability to see specialists costs and out-of-network coverage.
When it comes to health insurance you have your choice of several plan types. PPO may refer to. This means that you can use any hospital or see any doctor or specialist.
This system is broadly called managed care. What does PPO stand for in Insurance. PPO stands for Preferred Provider Organization.
Prisons and Probation Ombudsman. Generally speaking an HMO might make sense if lower costs are most important and if you dont mind using a PCP to manage your care. 1 PPOs are a type of managed care health insurance plan like their distant cousins health maintenance organizations or HMOs.
25-Diphenyloxazole an organic scintillator. Periodical Payment Orders PPOs This Working Party investigates Periodical Payment Orders PPOs and their effects on the UK insurance and reinsurance industry PPOs are a significant feature of insurers and reinsurers balance sheets already and are having an impact on pricing and capital modelling efforts of GI actuaries. Protoporphyrinogen oxidase an enzyme.
It stands for preferred provider option network. A PPO may be better if you already have a doctor or medical team that you want to keep but who dont belong to your plan network.