Most PPO benefit plans require the member or provider to pre-certify inpatient hospital admissions acute care inpatient rehab etc. Psychiatric Residential Treatment Request Form.
Https Www Bcbst Com Providers Forms Predetermination Form Pdf
Fax This Form to.

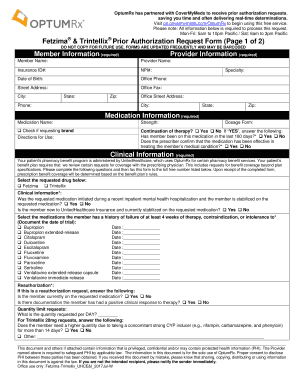
Bcbs tennessee prior authorization form. Magellan Health Services will provide a response within 24 hours upon receipt. To find a prior authorization form visit our forms page or click on the links below. Non-formulary drugs Part D reviewed by ESI.
For ERS or TRS participants refer. Mental Health Inpatient Request Form. Most preauthorization requests can be resolved by contacting Provider Relations and Servicing or PRS and requesting member benefits.
Applied Behavior Analysis ABA Assessment Initiation and Continuation Request Form. Weekdays from 8 am. Behavioral Health Patient Authorization Forms.
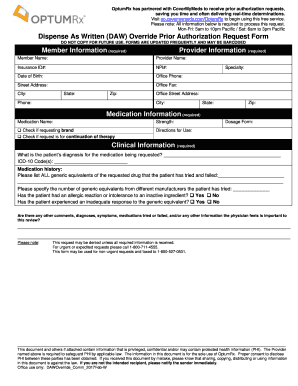
Office drugs prior authorization request PDF 301 KB. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Mental Health Outpatient Request Form.
Musculoskeletal prior authorization is required for spinal surgery joint surgery hip knee and shoulder and pain management. Psychological Testing Authorization Request Form Commercial Substance Abuse Clinical Service Authorization Request Form. Or download the PA and ST program criteria summaries and fax forms from the Prime Therapeutics website using the following links.
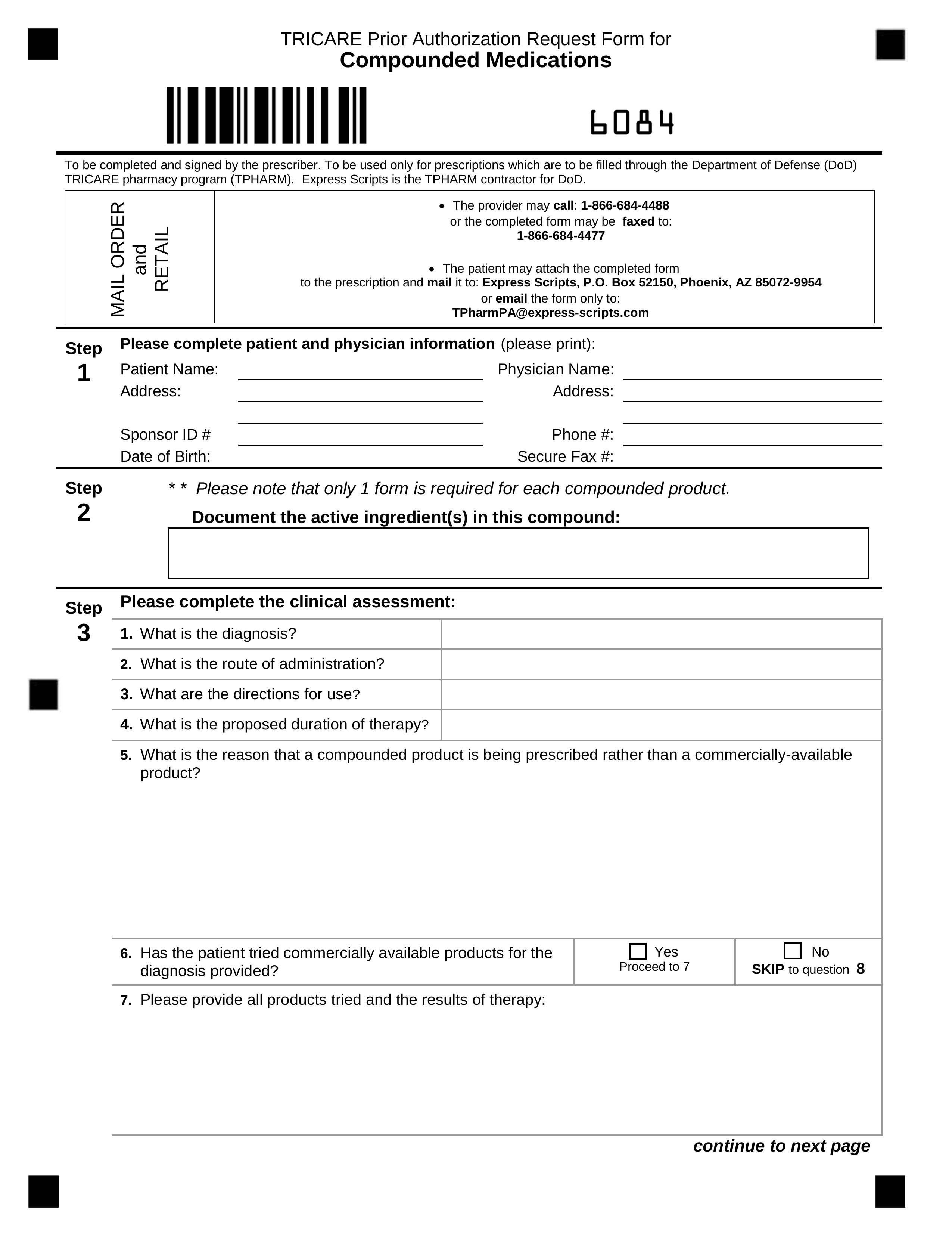
TennCare Pharmacy Program co Magellan Health Services 1st floor South 14100 Magellan Plaza Maryland Heights MO 63043 Phone. A prior authorization is not a guarantee of. Prior Authorization Request Form.
Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. 17 Zeilen Behavioral Health for Other BCBSTX Plans.
Blue Cross Blue Shield of Michigan Request for Preauthorization Form. BlueCross BlueShield of Tennessee 1 Cameron Hill Circle Chattanooga TN 37402. Commercial Substance Abuse Clinical Service Authorization Request Form.
Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. Physicians can access complete and submit PA and ST program criteria summaries and request forms electronically from the CoverMyMeds website. Transcranial Magnetic Stimulation TMS Pre-Authorization Request Form.
Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB Prescription drug prior authorization and step therapy exception request forms. Medical Policy and Pre-certificationPre-authorization Information for Out-of-Area Members To view the out-of-area Blue Plans medical policy or general pre-certificationpre-authorization information please select the type of information requested enter the first three letters of the members identification number on the Blue Cross Blue Shield ID card and click GO. Requests for the following services can be made by fax or mail.
Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Behavioral Health Levels of Care Program Descriptions.
BlueCross BlueShield of Tennessee. Blue Cross PPO Commercial Forms Use these forms to obtain prior authorization for administering medications in physicians offices and outpatient hospitals including urgent care hospital-based infusion care centers and clinics where the drug is injected or infused and billed on a UB04 or CMS 1500 form. Behavioral Health Out of Network Request Form.
Tennessee Medicaid Prior Authorization Form. Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts Medical policy precertification and preauthorization router. However if you would like to submit a request for preauthorization after contacting PRS you may submit a written request by completing this form.
Applied Behavior Analysis ABA Assessment Initiation and Continuation Request Form. Also known as preauthorization or pre-notification pre-certification confirms that a physicians plan of treatment meets medical necessity criteria under the applicable health benefit plan. Commercial Psychiatric Clinical Service Authorization Request Form.
Submit an electronic prior authorization request.