Appeal Form PDF File. Document your E-Visits for reimbursement.
Https Www Nebraskablue Com Media Files Nebraskabluedotcom Providers Forms Claims And Benefits Appeal Request Provider Fillable 4626 Ashx
If youd like to make a complaint or file an appeal about a claim that was denied call customer service at the number on the back of your member ID card.
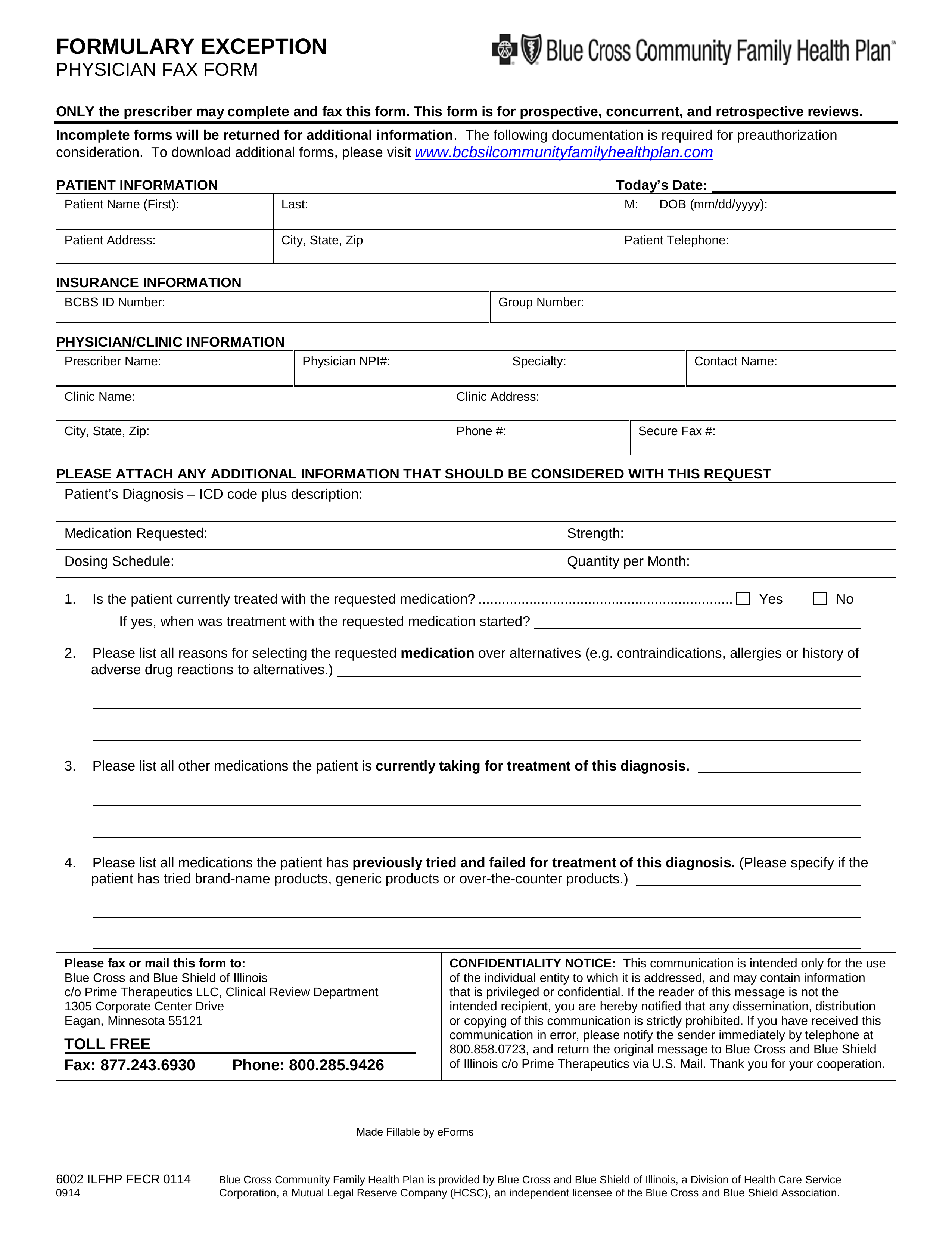
Blue cross blue shield appeal form. Blue Cross Blue. You can mail your appeal request form to. If you are unable to resolve your complaint you can file an appeal.
An Independent Licensee of the Blue Cross and Blue Shield Association 5 L_CC3 Appeal Form 20 01_14_20 After your appeal is filed with BCBSNM we will send you a letter within five business days. Medical forms for Arkansas Blue Cross and Blue Shield plans. Blue Dental Out-Of-Network Claim Form PDF File.
Provider Reconsideration Form Use this form to request review of a claim that has processed with an adverse determination. Blue Cross NC Providers. Use this form to grant Blue Cross and Blue Shield of Massachusetts permission to make a single.
Form to record your notes from ambulance trips. Please submit requests to the Appeal Department at. Availity LLC is an independent company providing claims administration services.
Notify Blue Cross NC of a change in your secured electronic channel vendor. Use these forms for Arkansas Blue Cross metallic and non-metallic medical plans members only. Medical appeals Dental appeals.
Start by downloading the complaintappeal form for your health plan. Spanish Version PDF File. When Arkansas Blue Cross and Blue Shield denies a claim for benefits the member receives a Personal Health Statement PHS or Explanation of Benefits EOB explaining the reason for the denial.
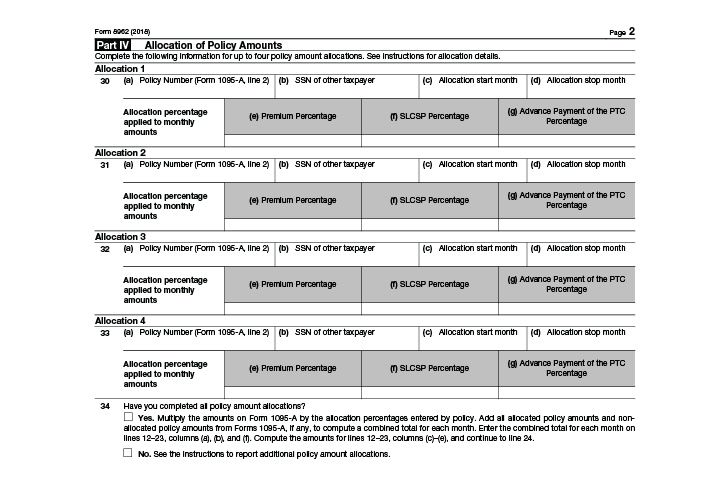
This form will allow the Appeals Department to process the appeal request promptly and efficiently. Fax us this form when a hospice patient has been or may be denied a medication at the pharmacy or to communicate a beneficiarys change in hospice status. Please review the instructions for each category below to ensure proper routing of your appeal.
Blue Cross Blue and Shield of New Mexico. Provider Appeal Form Instructions. We will respond to your appeal for a post-service claim within 60 days of when we receive your request and within 30 days for a.
English Version PDF File. Appeals are divided into two categories. Blue Cross and Blue Shield of Minnesota and Blue Plus are nonprofit independent licensees of the Blue Cross and Blue Shield Association.
The physicianclinical peer review process takes 30 days and concludes with written notification of appeal determination. Member Submitted Claim Form PDF File. 5373 Appeal Form Post Service Medical Necessity Decision Use this form to appeal a claim determination involving a post service medical necessity decision made by Horizon BCBSNJ.
Use this form to appeal or dispute a rejected BlueCard claim. It ensures the medical information and supporting documentation you fax or mail gets to the right area at BlueCross. You can submit up to two appeals per denied service within one year of the date the claim was denied.
You may use the appeal request form or call us at BCBSTX customer service at 1-888-657-6061 TTY 711. When you file an appeal BCBSTX will take another look at your case to see if there is something else we can do to solve your problem. Claim Reconsideration Request Form pdf Continuation of Care Election.
Blue Dental Extra Dental Cleaning Enrollment Form PDF File If your plan offers a 3rd annual cleaning and you are pregnant or have diabetes you can use this form to apply. These companies are Independent Licensees of the Blue Cross and Blue Shield Association. Florida Blue and Florida Blue HMO do not discriminate on the basis of race color national origin disability age sex gender identity sexual orientation or health status in the administration of their plans including enrollment and benefit.
Forms are available at the bottom of this page. Blue Cross and Blue Shield of Texas. Physicians and Providers may appeal how a claim processed paid or denied.
Blue Shield Final Provider Appeal and Resolution Office PO. Blue Cross Blue Shield Global Claim Form. Dialysis Erythropoietin EPO Appeal Request Form Use this form when providing medical documentation to support medical necessity dosage given.
To initiate a final Appeal providers and capitated entities must within 65 working days of Blue Shields initial determination or the time specified in the providers contract whichever is greater submit a written request to. For Dental Blue 65 members use the Dental Blue 65 Enhanced Dental Benefit Enrollment Form. The member has the right to file an appeal to request review of the denial of a claim in whole or in part.
Albuquerque New Mexico 87125-7630. All appeal decisions will be sent to you in writing and will include a detailed explanation about the decision. This is a library of the forms most frequently used by health care professionals.
The Designation of Authorized Representative for Appeal form and attach it to your appeal request. Box 629011 El Dorado Hills CA 95762-9011. Authorization Form for ClinicGroup Billing pdf Use for notification that a practitioner is joining a clinic or group.
Complete this form to begin the provider appeal process. Is a prerequisite for filing an Administrative. A routing form along with relevant claim information and any supporting medical or clinical documentation must be included with the appeal request.
To submit an appeal send us the Request for Claim Review Form within one year of the date the claim was denied. Use this form to begin the appeals process for Medicare providers. An appeal must be submitted in writing.
The appeal will be completed according to. Blue Cross Blue Shield of MA Provider Appeals PO Box 986065 Boston MA 02298. HealthSelect is administered by Blue Cross and Blue Shield of Texas PhysicianProfessional Provider FacilityAncillary Request For Claim AppealReconsideration Review Form Do not attach claim forms unless changes have been made from the original claim that was submitted.