Log into your CoverMyMeds account to create new manage existing and access pharmacy-initiated prior authorization requests for all medications and plans. Type to chat with us or call us at 866-452-5017.
 Covermymeds Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Covermymeds Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
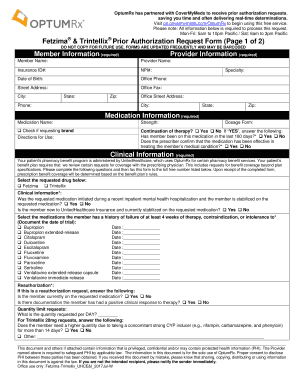
Prior authorizations PA play an important role in maximizing the clinical benefit of pharmacy care minimizing patient exposure to unnecessary health risk and reducing waste.
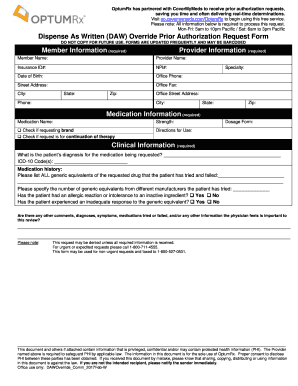
Covermymeds prior auth. To submit a prior authorization click the Submit Prior Auth button in PROscripts. Complete and submit to plan. It asks the necessary questions and puts them all in one place.
Much of the patient medication and prescriber information will be filled in. Humana Medicare Prior Auth Form For Medication Express Scripts Prior Auth Form Unique Humana Prior Authorization Form Best Medicare Part D Prior Covermymeds Prior Authorization Form Pdf. Our electronic prior authorization ePA process through CoverMyMeds is the preferred method to.
CoverMyMeds automates the prior authorization PA process making it a faster and easier way to review complete and track PA requests. The user can then enter the necessary patient and prescription details within the integrated CoverMyMeds application and submit the PA. Sign up CoverMyMeds The Leader In Electronic Prior Authorization.
While reviewing the prescription change request from the pharmacy the user should click the Prior Auth button on the bottom action row of the Send Rx screen. This button is accessible on all claim rejection screens. Complete the remaining fields and submit to the.
It is now used for a lot of medication PAs but prior authorizations have a larger scope than the pharmacy benefits section of a health plan. The prior authorization PA process can present patients with unique access challenges depending on the relative complexity and expense of their prescribed medications. CoverMyMeds can be started in any setting as long as you have an account but if you dont have all the clinical information passing the started prior authorization.
Solving Prior Authorization Providing a safety net for medications requiring prior authorization PA from the point of prescribing to the pharmacy counter. Helping Patients 37 of PA-related claim rejections are abandoned at the pharmacy. CoverMyMeds automates the prior authorization PA process making it a faster and easier way to review complete and track PA requests.
OR FAX this completed form to 855 554-5233. 75 of EHRs Integrated. CoverMyMeds is AzCHs preferred way to receive prior authorization requests.
Once the response is received within the integrated ePA solution the user can add the authorization. CoverMyMeds Prior Authorization Software Complete Your Patients Prior Authorization Request Enter the key from the prior authorization PA fax you received to complete the request online and help your patient get the medication they need. If a PA was started by a pharmacy it will appear in your dashboard.
_ Click to Chat with CoverMyMeds. Form must be fully completed to avoid a processing delay. CoverMyMeds is an online platform that submits insurance claims.
This report details various aspects of the PA process and associated difficulties for patients along with innovations from CoverMyMeds which can assist patients throughout the medication access journey. Our electronic prior authorization ePA solution is HIPAA compliant and available for all plans and all medications at no cost to providers and their staff. Our electronic prior authorization ePA solution is HIPAA compliant and available for all plans and all medications at no cost to providers and their staff.
CoverMyMeds automates the prior authorization PA process making it a faster and easier way to review complete and track PA requests. CoverMyMeds ePA is available in iPatientCare. While E-Prescribing ensure the Start PA box is checked.
CoverMyMeds will use the plan and rejection data to select the proper form auto populate the necessary fields and then electronically share the request to the prescriber for completion. View the Prior Authorization task list under Tools Click the 6-digit ID. Patients Name Last First MI.
For Prior Authorization Status Call. Our electronic prior authorization ePA solution is HIPAA compliant and available for all plans and all medications at no cost to providers and their staff.
