In vitro fertilization IVF. Hello Were happy to check on your plans coverage for infertility services if youd like to send us a private message with your plan ID and contact information.
 Insurance Coverage Fertility Solutions Ne
Insurance Coverage Fertility Solutions Ne
Health Care Coverage 1-to-1 Videos.
Bcbs ivf coverage. While IUI is addressed in this. However Blue Cross Blue Shield is a national federation of affiliated companies using this trade name. Our most expensive IVF medication cycle was 285.
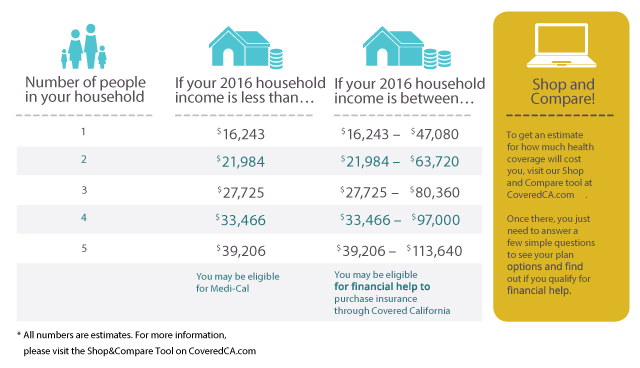
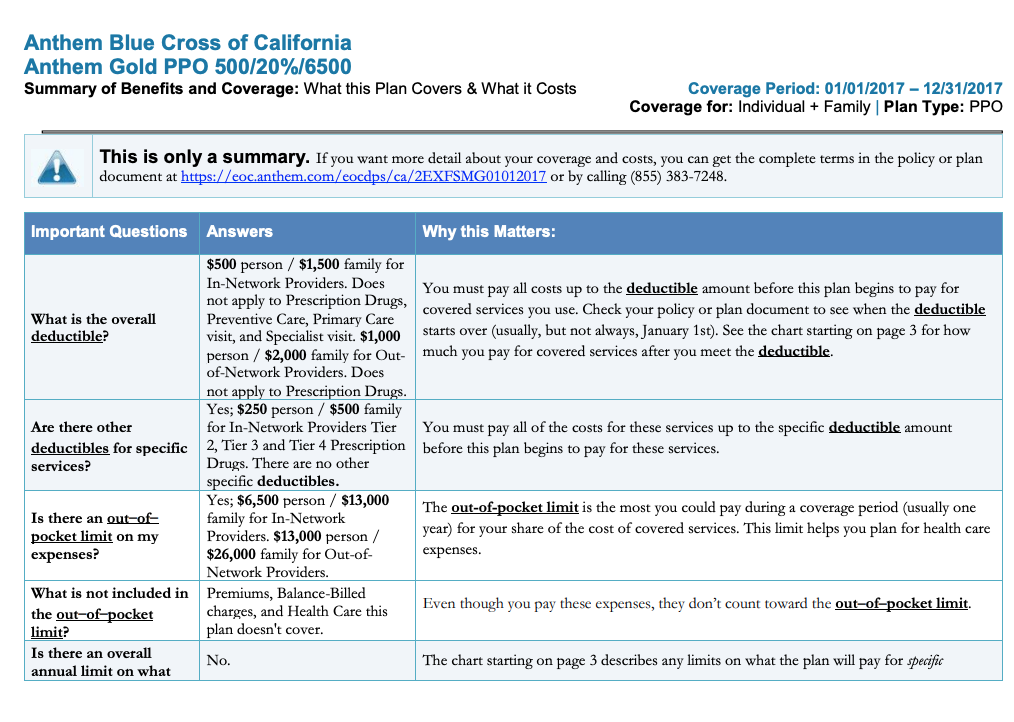
NCQA is not affiliated with Blue Cross Blue Shield of Massachusetts or CMS nor is the award given or endorsed by Medicare. Individual. Length of time necessary for women under age 35 remains at 1 year.
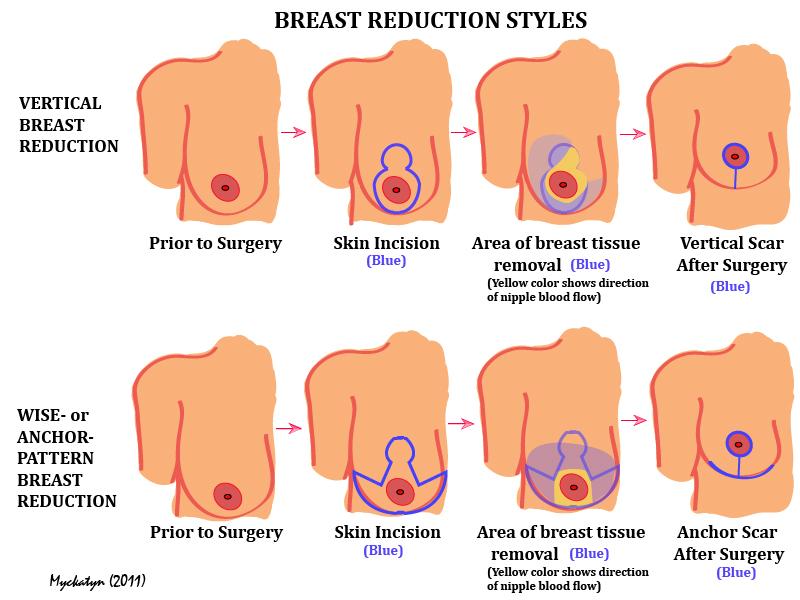
The policy addresses medical necessity criteria and coverage guidelines related to the treatment of female infertility using assisted reproductive technology such as artificial intrauterine insemination IUI or in vitro fertilization IVF. Blue CrossBlue Shield of Texas completely covers the medications that are required for infertility treatment. All that the patient must be concerned with is the co-payment at the time of purchase.
Normally it would have been a few thousand. How Health Insurance Works. This section applies to plans offered by Blue Cross Blue Shield of.
Importance of Health Insurance. Covered Infertility Benefits up to the lifetime maximum None Infertility Benefits Blue Shield Payment Covered Infertility Benefits up to the lifetime benefit maximums as described in this Supplement 50 of the Allowable Amount 1 Infertility Benefits are only covered when provided by Preferred or Participating Providers. These services are only covered if the members benefit booklet identifies Artificial insemination AI Intrauterine Insemination IUI andor In Vitro fertilization IVF as covered services.
Blue Distinction Centers for Fertility Care focus on in vitro fertilization IVF. Blue Cross Blue Shield BCBS will sometimes issue plans that cover infertility treatment including IVF when required by state law or when requested by an employer group. Please check the member benefit language regarding the benefits for artificial means of conception.
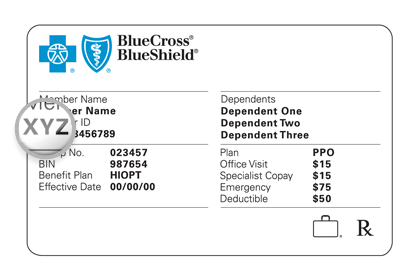
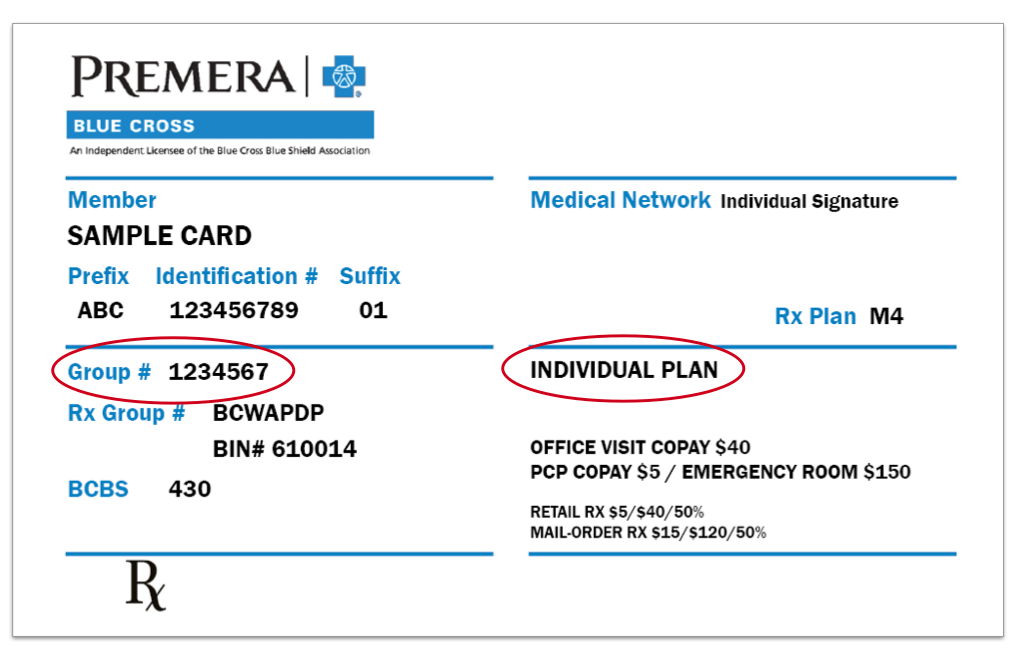
To find out which services are covered under your policy at any facility please call the customer service phone number on the back of your Blue Cross and Blue Shield of Texas member ID card. Coverage for members undergoing a treatment other than chemotherapy that is expected to render them permanently infertile excluding voluntary sterilization. This voluntary program is open to IVF ART providers in various care settings including individual physicians physician groups and clinics.
Blue Cross Blue Shield of Massachusetts Medicare Advantage PPO Plan and Medicare Advantage HMO Plan are rated 45 out of 5 overall nationally. O One cycle of IVF with egg or embryo cryopreservation if the member is. Associated donor medical expenses are also covered including but not limited to physical examinations laboratory screenings psychological screenings and prescription drugs.
Blue Distinction Centers for Fertility Care focus on in vitro fertilization IVF which is the most common assisted reproductive technology ART treatment and is widely becoming the preferred option for fertility treatment. DIRECTORY OF BLUE DISTINCTION CENTERS and BLUE DISTINCTION CENTERS FOR FERTILITY. Womans partner or a sperm donor.
Are frequently excluded from coverage. This is a valuable part of the coverage as the medication cost for most infertility care is the most expensive part of the treatment. It did help with IUIs though and we had awesome drug coverage that saved us quite a bit.
We ha be Blue Cross Blue Shield and it has a lifetime infertility coverage of 10000 but IVF is not covered at all. It will focus on in vitro fertilization IVF which is the most common assisted reproductive technology ART treatment and is widely becoming the preferred option for fertility treatment. In most instances ART will involve in vitro fertilization IVF a procedure in which oocytes harvested from the female are inseminated in vitro with sperm harvested from the male.
The maximum number of completed oocyte retrievals that are eligible for coverage under this Policy in your lifetime is six. Expands the existing infertility mandate to require coverage for women over age 35 who are unable to conceive for at least 6 months. Footer Skip to footer content.



/invisalign-and-dental-insurance-coverage-7565b48f924b43c7b9f7f7431be4dcbe.png)