This is the highest copayment tier and includes some generics and brand-name covered drugs not selected for Tier 2. Level or Tier 2.

Knowing what tier your drug is in together with looking at your plans benefits can help you predict how much that drug will cost.
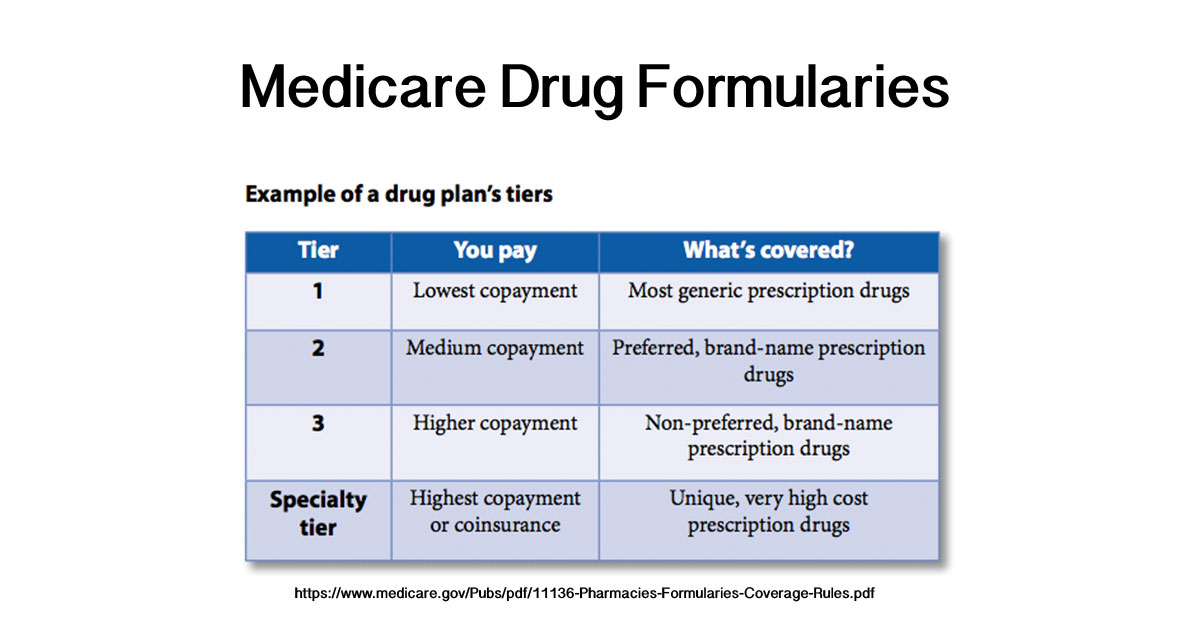
Drug formulary tiers. Tier 1 Preferred generic drugs lowest cost-sharing. This formulary will tell you what tier your drug is in. A tiered formulary divides drugs into groups based mostly on cost.
These categories are called tiers. Level or Tier 1. Brand-name drugs including preferred and nonpreferred options.
Each plan decides which drugs on its formulary go into which tiers. Drugs are placed in tiers based on the type of drug. DRUG FORMULARY This formulary was updated on 04202021.
Non-preferred generic and non-preferred brand name drugs. For example a plan with five drug formulary tiers might have these levels. Each tier will have a defined out-of-pocket cost that the patient must pay before receiving the drug.
Generic preferred brand non-preferred brand and specialty. Tier 5 Specialty drugs highest cost-sharing. Medications from the drug formulary are placed on tiers.
Your health plans formulary is divided into three or four categories. Many common brand name drugs called preferred brands and some higher-cost generic drugs. Drugs from our formulary or add prior authorization andor quantity limits on a drug or move a drug Updated 102020 ii to a higher cost-sharing tier we must notify affected members of the change at least 30 days before.
However since the plans are offered by private insurers you also find five- and six-tier systems. Drugs in lower tiers generally cost less than drugs in higher tiers. Tier 3 Preferred brand-name drugs.
When you fill a prescription the amount you pay depends on the coverage stage youre in. Formularies can have a single tier where all drugs have the same cost to patients or multiple tiers where cost varies. You should contact us to ask us for an initial coverage decision for a formulary tiering or utilization restriction exception.
Members will have the lowest cost share with a Tier 1 medication so consider prescribing a generic Tier 1 medication when appropriate. The formulary is usually divided into tiers or levels of coverage based on the type or usage of the medication. Many Medicare prescription drug plans use a four-tier system.
This tier includes many generic drugs. When you request a formulary tiering. A plans formulary might have three four or even five tiers.
Heres what typical formulary tiers look like. A Medicare formulary may categorize prescription drugs into five tiers. Your drug payment stage.
You should contact us to ask us for an initial coverage decision for a formulary tiering or utilization restriction exception. Drug payment stage and drug tiers The amount you pay for a covered prescription drug will depend on. Preferred brand drugs and select insulin drugs.
Generic drugs which could be low-cost preferred generics or general preferred generics. Prescription Drug Formulary. Your drugs tier.
Tier 4 Non-preferred brand-name drugs. Level or Tier 3. Medications on this tier have the lowest copayment.
Covered prescription drugs are assigned to 1 of 4 different levels with corresponding copayment or coinsurance amounts. Lower-cost commonly used generic drugs. Each covered drug is in 1 of 5 drug tiers.
Medications on this tier are subject to the middle copayment. What Are Drug Tiers. In general the lowest-tier drugs are the lowest cost.
Covenant Advantage HMO-POS Covenant Advantage Plus HMO-POS. Most generic medications are included on the PDL as Tier 1 medications. For more recent information or other questions please contact BayCare.
When you request a formulary tiering. A drug tier is a group of medications included within a similar price range. A drug formulary is a list of generic and brand name drugs that are preferred by a health plan based upon their effectiveness and cost-savings.
The lowest tier has the lowest prices with costs rising along with the tiers. Your plan has different stages of drug coverage. Medicare formulary tiers The amount you pay for a prescription drug may depend on which tier your drug is on and whether you fill your prescription at a network pharmacy.
Under a healthcare plan the list of covered prescription drugs is called a formulary. Tier What drugs are included. Check your benefit summary to see what your cost- share is for the drugs in each tier.
Tier 2 Non-preferred generic drugs. This tier includes some generics and brand-name drugs. Note that when a brandname - medication becomes available as a generic that brandname product may move to - a higher tier.
