Healthy Moms Healthy Babies. PROVIDER INFORMATION REQUIRED Provider Name.
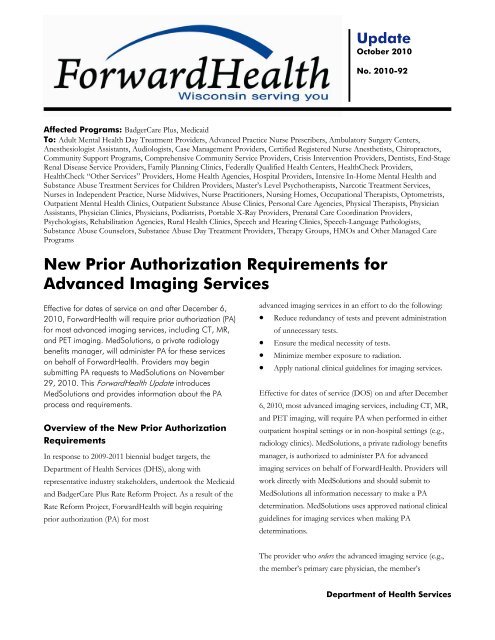 New Prior Authorization Requirements For Advanced Imaging Services
New Prior Authorization Requirements For Advanced Imaging Services
Players Streets Players Have Famous To Other Cars Prior Another In Medsolutions Games Racing To That Opportunity Their Auth Fact Their And Why Online Ideal Is The People Cause Opposition Enjoy The On Prefer Its also good to make a mental note of the injury.
Med solutions prior auth. Radiology Prior Authorization Request Form. Home - Elixir Solutions Prior Authorization Portal. Medica Prior Authorization and Notification Requirements Service Category Policy Name Current Procedural Terminology CPT Codes Advantage Commercial products----- Solution Individual Family Business IFB products ----- Medica Health Plan Solutions MHPS Medica Advantage HMO HMO-POS and PPO Medica Solution.
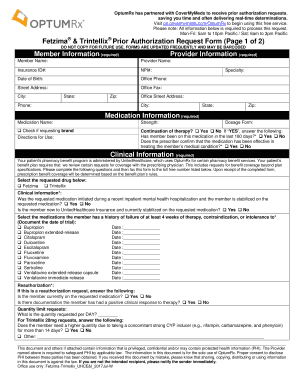
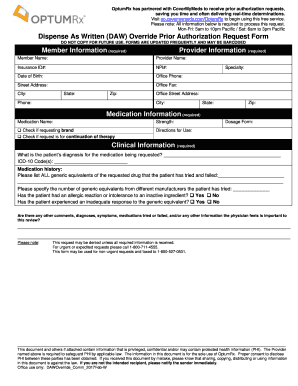
Dont have an account. You may submit a prior authorization request through our online provider center or complete a Prior Authorization Form PDF. Prior authorization is necessary to ensure benefit payment.
855 247 3233 Section I General Information Review Type Non Urgent Urgent Clinical reason for urgency Request Type Initial. PARx Solutions Full Prescribing Information Important Safety Information. To better serve our providers business partners and patients the Cigna Coverage Review Department is transitioning from PromptPA fax and phone coverage reviews also called prior authorizations to Electronic Prior Authorizations ePAs.
Process quickly due to date of Servicescheduling constraints Pre-Scheduled date of Service_____ Auth Date needed by_____ Definition of. Sucraid sacrosidase is an oral enzyme replacement therapy indicated for the treatment of genetically determined sucrase deficiency which is part of congenital sucrase. This information can be obtained by contacting your prescribing physician.
Log in to take your Health. Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptionsA non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State. Provider Prior Authorization Request Line.
Medical Prior Authorization Request For m. Prior AuthorizationReferral Requirements Effective. Helping Patients Get the Medication They Need to Live Healthy Lives.
EviCore will provide a voice message service for telephone requests received outside the normal operating hours of 8 am. Summary of Drug Limitations. For Applied Behavioral Analysis.
Requests from each of these mechanisms are routed through the same process internally at MedSolutions for determination. Requests may also be. Here are some of the key highlights of.
All fields are REQUIRED. Contact Us for Sales or Inquiries. An incomplete request form will delay the authorization process Standard Request Standard RequestQuick Response.
By phone by fax and online. Failure to provide all relevant information may delay the determination. Enroll today and get your own Registered Nurse Health Coach.
Before you get started in addition to your insurance card you will need the following information. Specialty Drug List Prior Authorization. Date of injury what you were doing how it happened what force and what angle was the force directed and.
As part of this effort we retired certain fax numbers for medical prior authorization requests in 2019 and asked you to use the Prior Authorization and Notification tool on Link the same website you use to check eligibility and benefits manage claims and update your demographic information. MEMBERPATIENT INFORMATION REQUIRED Name. Full Prescribing Information Important Safety Information.
Join today and start your journey to a lifetime of wellness and joy for you and your baby. Three Ways to Obtain Prior Authorization from MedSolutions for Radiological Services For your convenience MedSolutions offers three mechanisms to initiate a prior authorization request. All Non-Par Provider Requests Requires Authorization Regardless of Service.
MEDICAL PRIOR AUTHORIZATION REQUEST FORM - PLEASE FAX FORM TO. Prior authorizations will be accepted 24 hours a day seven days a week excluding planned down time for system maintenance through the eviCore website or by phone at 888 693-3211 or fax to 888 693-3210. If there are any inconsistencies with the medical office records please elaborate in the comment section.
812 -378 7054 Phone. Program Prior AuthorizationMedical Necessity Medication Sucraid sacrosidase oral solution P. Watch Video about using PARx the free streamlined and HIPAA-secured PA solution for physicians to help patients get the medication they need.
Contact your office administrator to get started. On the prior authorization form the person making the request must provide a medical rationale as to why the chosen. You may prescribe a health care service treatment equipment or medication to your patient which requires prior authorization.
Get An MCM Health Coach Today. Learn more about retired medical prior authorization fax numbers. EPAs save time and help patients receive their medications faster.
For NON-URGENT requests please fax this completed document along with medical records imaging tests etc. Medical Services Require Prior. Solutions for Better Health For You Your Members and Your Bottomline.
Cover My Meds PARx.