Tier 3 medications are non-preferred traditional medications. Tier 4 interventions comprise residential specialised drug treatment which is care planned and care co-ordinated to ensure continuity of care and aftercare.
Follow the steps below when asking for a tiering exception.

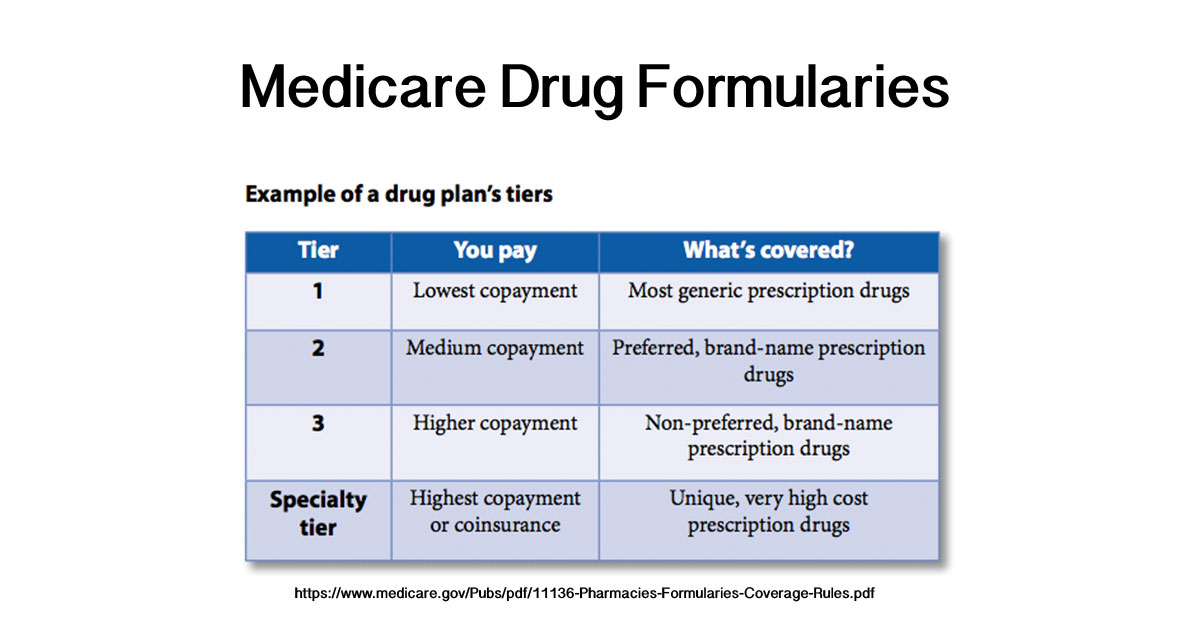
What is a tier 4 drug. These drugs will cost you a significant amount out-of-pocket. This is the highest copayment tier and includes some generics and brand-name covered drugs not selected for Tier 2. Some health plans have more than four tiers and others have only two or three but they all work the same.
Members will have the highest cost share for Tier 3 medications unless the medication is a specialty medication and is designated as Tier 4. If you qualify for Extra Help paying for your prescription drugs your copays and coinsurance may be lower. Tier 1 medications are your lowest-cost options.
Your out-of-pocket cost will be highest in tier 4. JAH March 2007 Tier 4 interventions. Medications on this tier are subject to the middle copayment.
4 rijen Tier 4 These drugs are considered specialty drugs and are typically used to cover serious. This is how much you will pay when you fill a prescription. Non-Preferred Brand Tier 4 Preferred Specialty Tier 5 and Non-Preferred Specialty Tier 6.
Your physician may have the option to write you a prescription for a Tier 1 Tier 2 Tier 3 or Tier 4 drug as defined below. Medications on this tier have the lowest copayment. Based on your benefit design drugs can either be in these tiers or you may have fewer tiers eg all generics in one tier.
Instead youll pay a percentage of the total cost. How do I find my formulary. Each tier is assigned a cost which is determined by your employer or health plan.
If your medication is placed in Tier 2 3 or 4 look to see if there is a Tier 1 option available. Tier 4 Tier 4 medications are non-preferred specialty medications. Tier 4 includes generics preferred brands non-preferred brands and specialty drugs.
This is how much you will pay when you fill a prescription. If you are charged a high copay at the pharmacy talk to. The most expensive tier usually occupied only by speciality drugs such as newly approved drugs.
However there may be instances when only a Tier 4 drug is appropriate which will require a. Tier 4 is where you find prescriptions with the highest cost mostly specialty drugs. If your medication is placed in Tier 2 3 or 4 look to see if there is a Tier 1 option available.
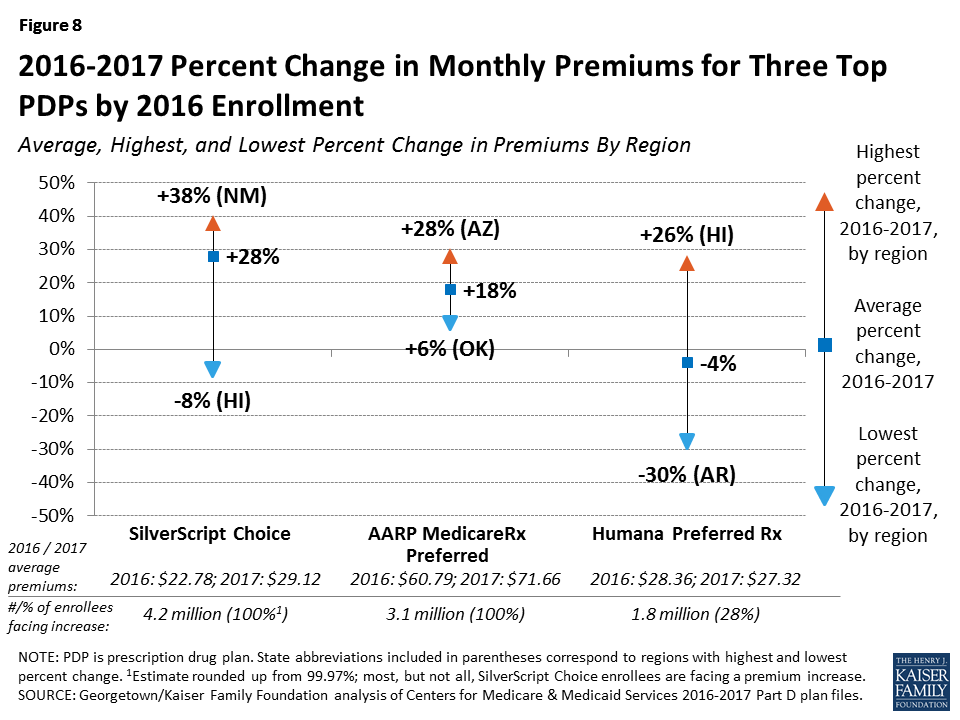
Medicare plans with prescription drug coverage organize medications into different price categories called tiers Medicare plans can have as many as 4 or 5 tiers and generally drugs in the lower tiers have lower costs while drugs in higher tiers have higher costs. All covered drugs are placed into one of four tiers. Specialty medications treat rare or serious medical conditions.
Tiers are the different cost levels you pay for a medication. Non-preferred and expensive brand-name drugs are usually in this tier. How Are Drugs Priced on the Tiers.
Tier 1 medications are your lowest-cost options. Prescription drug pricing varies according to the insurer. Theyre the lowest-cost brand.
Non-Preferred Brand and Non-Preferred Specialty drugs are not listed in this document. For example a tier 1 drug will usually have lower copays than a tier 3 drug. Each tier is assigned a cost which is determined by your employer or health plan.
Tiers are the different cost levels you pay for a medication. Tier 2 will have non-preferred generics and on up as in the four-tier formulary. On five- and six-tier systems the first tier is preferred generics.
Non-preferred generic and non-preferred brand name drugs. This tier includes some generics and brand-name drugs. These drugs typically do not have a specific copay.
Tier 4 Non-preferred brand-name drugs Tier 5 Specialty drugs highest cost-sharing To get the most out of your prescription drug coverage note where your prescriptions fall within your plans drug formulary tiers and ask your doctor or prescriber for advice. This tier includes many generic drugs. Unique andor very high-cost brand and generic drugs.
For tiering exception requests you or your doctor must show that drugs for treatment of your condition that are on lower tiers are ineffective or dangerous for you. Drug specialist inpatient treatment and residential rehabilitation Definition. 6 rijen These are brand name drugs that dont have a generic equivalent.