The prior authorization must cover the entire date span and all services submitted on the claim to avoid requests for additional information and possible delays or denials. Frequently asked questions for providers document.
Https Member Carefirst Com Carefirst Resources Provider Pdf Drug C7019 A Mn Pa Md Pdf
A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
Blue choice prior authorization form. Please fax the completed form. HIPAA Authorization for Disclosure of Health Information authorizes Independence Blue Cross Independence to release members health information. Also includes the CAR-T Monitoring Program Givlaari Monitoring Program Luxturna Monitoring Program Onpattro Monitoring Program and Zolgensma Monitoring Program.
Once notified of admission medical information is applied against InterQual. A prior authorization is not a guarantee of benefits or payment. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Massachusetts Standard Form for Medication Prior Authorization Requests eForm or contact Clinical Pharmacy Operations. For members who have prescription drug coverage through Independence Blue Cross Independence prior authorization is required for certain prescribed formulary drugs in order for such drugs to be covered. Medicaid only BCCHP and MMAI.
However out-of-network providers are not contracted with us and have not agreed to accept this responsibility. Prior Rx Authorization Forms Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan.
Prior Authorization of Drugs Blue Cross Blue Shield of Rhode Island. Other medications that require prior authorization. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review.
Prior autorization south carolina Medicaid SCDHHS Medicaid health plan prior auth drug medicine Created Date. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Anthem has also made available a series of forms.
Link to the Concomitant Opioid Benzodiazepine Pediatric Behavioral Health Medication Hospital Outpatient Prior Authorization Opioid and Pain and Second-Generation Atypical Antipsychotic Initiatives. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. For questions contact the plan at the associated phone number.
The approval criteria were developed and endorsed by the Pharmacy and Therapeutics Committee and are based on information from the US. To obtain prior authorization for service categories not listed on this form please contact the members MCO directly for instruction. Requests will be confidentially reviewed according to payment criteria developed by Blue Cross in consultation with.
Prior Authorization is a pre-approval process to determine if certain prescription drugs will be reimbursed under a members benefit plan. Implant Reimbursement Request Form. LTACH and Skilled Nursing Facility Enhancement Assessment Form PDF Blue Cross PPO Request for Preauthorization Form PDF Medicare Plus Blue PPO.
Some services require prior authorization preauthorization before they are performed. 313- 908-6040 1- 833-217-9670 Fax intake forms. Select Health of South Carolina Subject.
MCO Universal Prior Authorization Form BabyNet A copy of the IFSP must be attached to the PA Request. Universal Prior Authorization Medication Form - Pharmacy - First Choice - Select Health of South Carolina Author. Failure to prior authorize may result in reduced payment or denial and health care providers cannot collect these fees from the members.
Medicaid Claims Inquiry or Dispute Request Form. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. Urgentemergency admissions do not require prior authorization.
Out-of-network services require prior authorization. We encourage you to verify that a Prior Authorization has been approved BEFORE you receive services or supplies that require a Prior Authorization. The terms of the.
Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members. Fax the COMPLETED form and the IFSP. Medicare Plus Blue PPO non-Michigan Skilled Nursing Facility Acute Rehabilitation Facility Fax Assessment Form PDF Medicare Plus Blue PPO LTACH Fax Assessment Form PDF.
Blue Choice members using their self-referred benefit do not need to get prior authorization. Authorization information Web intake. Provider Demographic Change Form Please submit this form to our Corporate Provider File Department when adding additional office locations to your practice or if your practice moves from its current location.
Which procedures require authorization through TurningPoint in the. Medicaid only BCCHP and MMAI Medicaid Service Authorization Dispute Resolution Request Form. HIPAA Personal Representative Request Form appoints another person as members personal representative.
Primary Care Physician PCP Change Form This is a form that providers will supply to the patientmember when they are changing their PCP. To request prior authorization for these medications please submit the. An in-network health care provider will request a prior authorization on your behalf.
Form Title Networks Expedited Pre-service Clinical Appeal Form.
 Blue Cross Blue Shield Prior Authorization Form Illinois Unique Prescription Refill Request Form Unique 10 Prior Authorization Form Models Form Ideas
Blue Cross Blue Shield Prior Authorization Form Illinois Unique Prescription Refill Request Form Unique 10 Prior Authorization Form Models Form Ideas
Https Provider Carefirst Com Carefirst Resources Provider Pdf Drug 1021 A Contour Test Strips Pdf
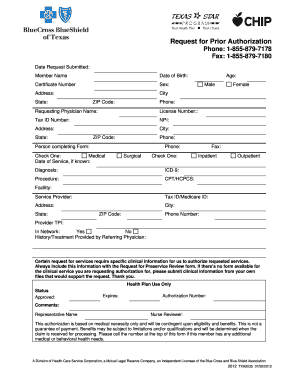 Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
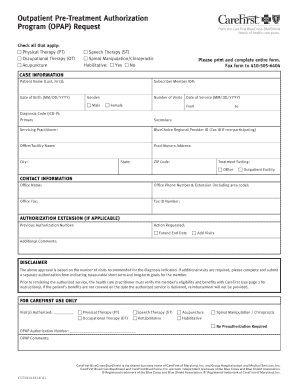 Fillable Online Carefirst Bluechoice Authorization For Mental Health Treatment Outpatient Form Fax Email Print Pdffiller
Fillable Online Carefirst Bluechoice Authorization For Mental Health Treatment Outpatient Form Fax Email Print Pdffiller
Https Member Carefirst Com Carefirst Resources Pdf Non Formulary Drug Exception Form Pdf
Https Individual Carefirst Com Carefirst Resources Pdf Forms Ma Prior Authorization Form Opap Pdf
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
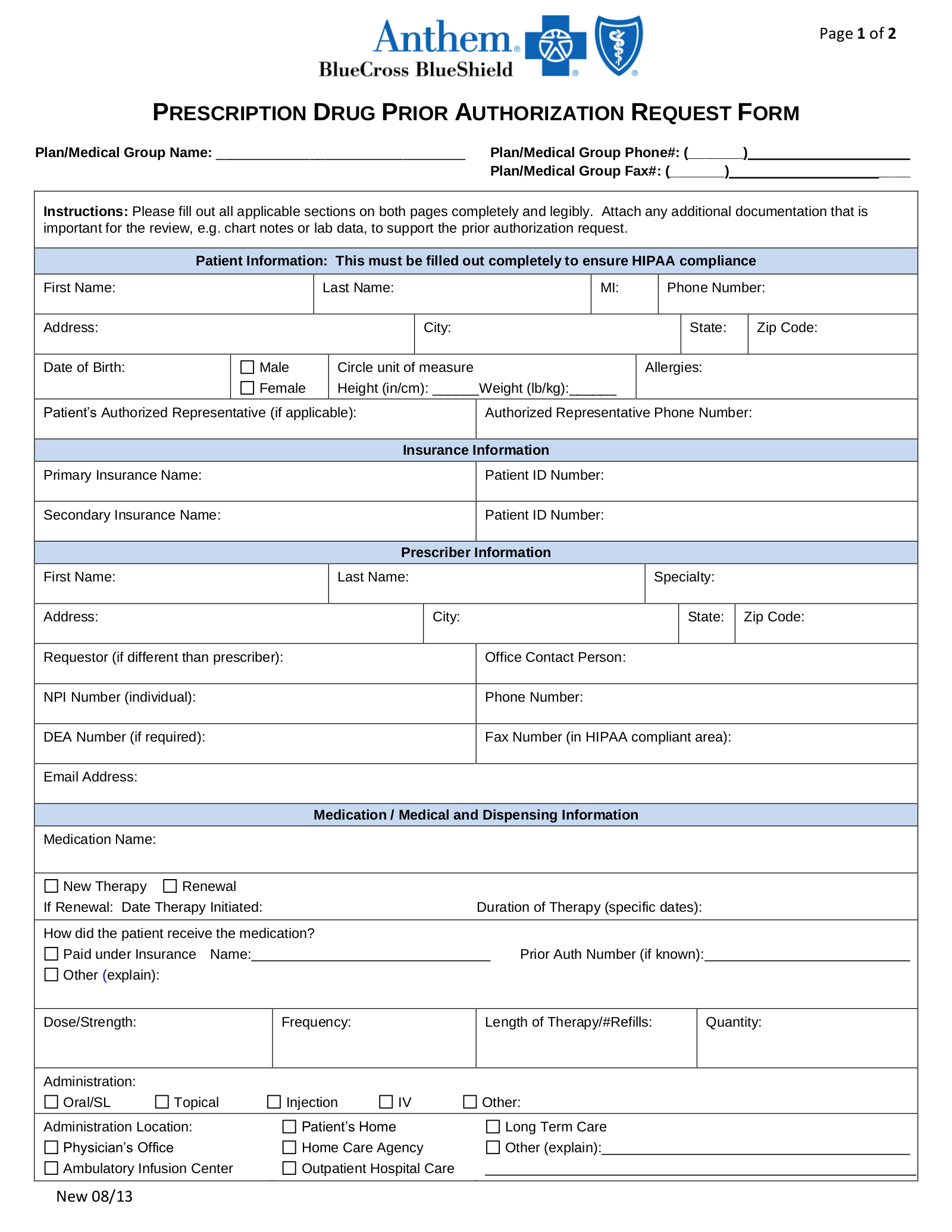 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
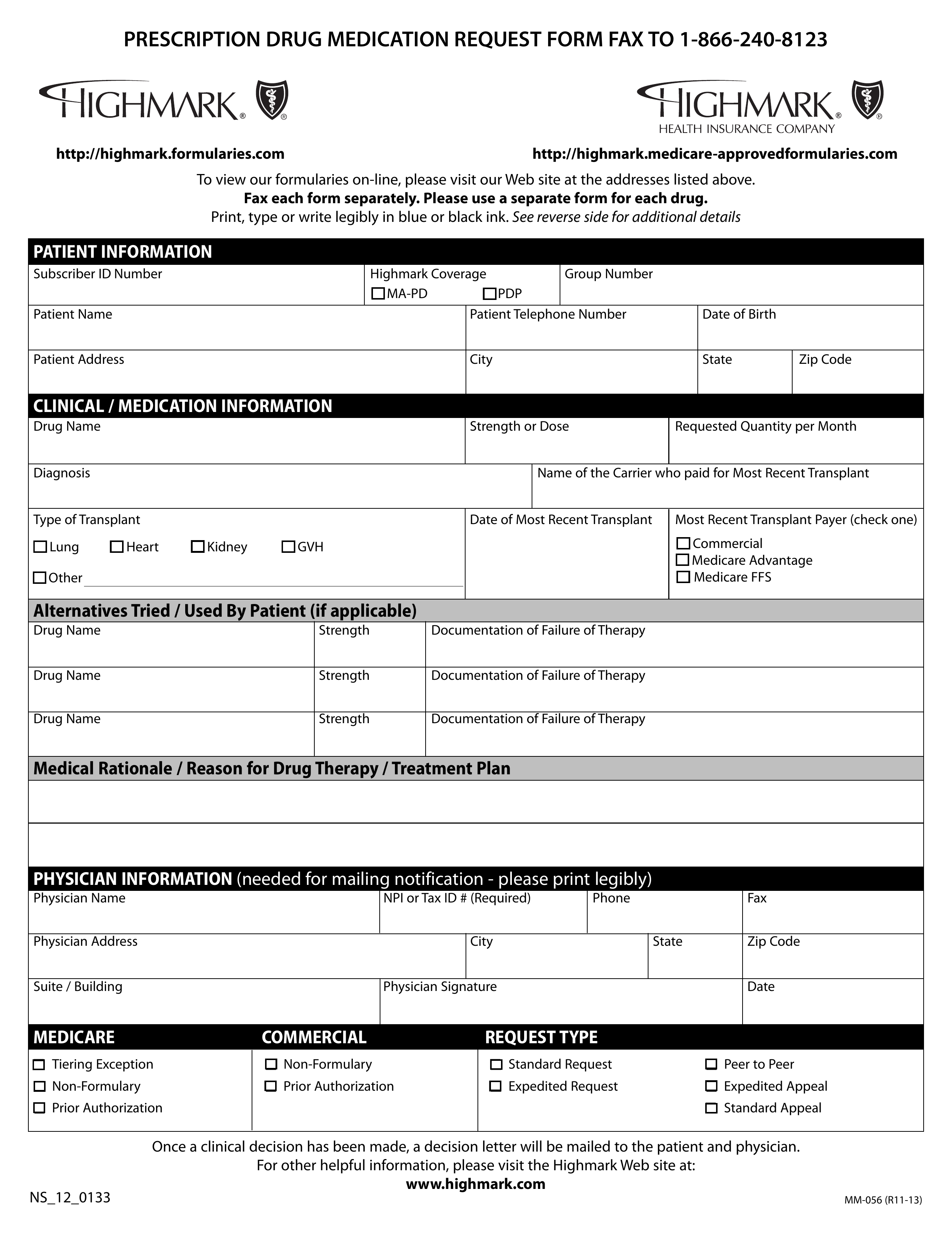 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
Https Www Bluechoicesc Com Sites Default Files Documents Providers Precertification Requirements Pdf
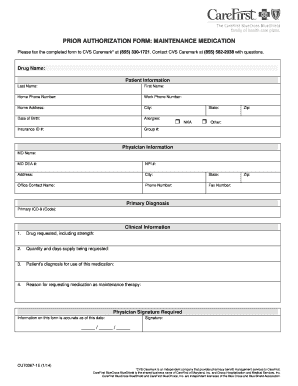 Fillable Online Prior Authorization Form Maintenance Drug Carefirst Fax Email Print Pdffiller
Fillable Online Prior Authorization Form Maintenance Drug Carefirst Fax Email Print Pdffiller
Https Provider Carefirst Com Carefirst Resources Provider Pdf Drug 288 C Subsys Pdf
Https Www Bluechoicesc Com Sites Default Files Documents Providers Priorauth Services Proceduresrev Pdf
 Florida Blue Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Florida Blue Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.