An Employers Guide to Health Continuation Coverage Under COBRA The Consolidated Omnibus Budget Reconciliation Act Source. Benefit Strategies LLC will notify the carrier andor employer of COBRA election upon receipt of completed enrollment paperwork and full initial payment.
However the act does not require them to pay for it.
How to get cobra paperwork. MS Word PDF. The Consolidated Omnibus Budget Reconciliation Act of 1986 COBRA amended the Public Health Service Act the Internal Revenue Code and the Employee Retirement Income Security Act ERISA to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations where it would otherwise be. A plan however may provide longer periods of coverage beyond those required by COBRA.
The employer or plan administrator then have evidence that the COBRA notice was actually mailed to the last known address of. The majority of Americans have private health insurance. I just started a new job that provides group health insurance so I am no longer eligible for the COBRA subsidy.
Learn more about COBRA which allows you to keep health insurance when your job changes unexpectedly. COBRA Premium Assistance under the American Rescue Plan Act of 2021 FAQs. This publication contains information about the COBRA premium reduction provisions of the American Recovery and Reinvestment Act of 2009 ARRA.
Cheaper options may be available in the public marketplace made. Change in Eligibility Q1. Model General Notice and COBRA Continuation Coverage Election Notice.
COBRA or the Consolidated Omnibus Budget Reconciliation Act is a federal law that gives employees the option to continue health insurance coverage after ending employment. Then when you receive your election notice from your insurance company review the price of your COBRA. COBRA law provides for up to 149 days before a COBRA participant qualified beneficiary is.
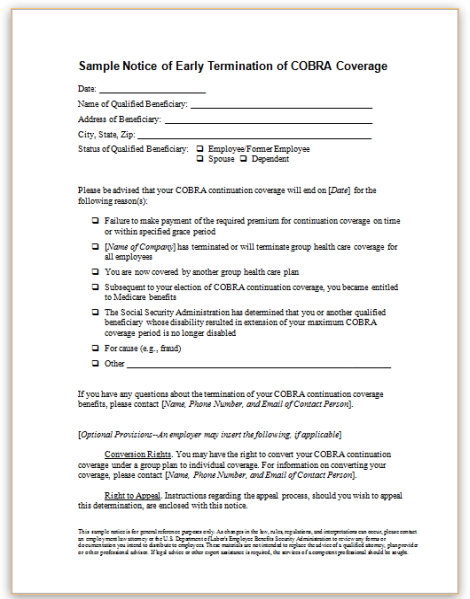
Early Termination Notice non-payment After the COBRA month closes and about a week passes to allow for mail time you will process the termination and issue a letter. Knowing the COBRA timelines and deadlines are critical to ensuring compliance. COBRA establishes required periods of coverage for continuation health benefits.
This process may take up to 5-10 business days after payment is received in this office. To sign up for COBRA insurance start by notifying your insurance company that youre eligible for COBRA through a qualifying event such as a divorce or job loss. Now that the we have discussed what COBRA is in general terms.
US Department of Labor Note. How do I notify my former employer that I should no longer receive the subsidy. The federal COBRA law requires certain employers to offer a continuation of group health coverage to employees who are losing their jobs either through termination by the employer a layoff or a resignation.
To fully understand COBRA head over to the US Department of Labors site here. More than 56 percent receive health insurance through their employer according to the US. Also available in Spanish MS Word PDF.
When does benefit coverage get reinstated or become active under COBRA. Always get your termination notifications in writing. General COBRA FAQs for Employers.
This publication has not been updated for recent amendments made to ARRA. COBRA is just one part of a much larger legal puzzle. COBRA requires employers to keep you on their insurance for as long as you need it or for the maximum time frame.
Changes in Plan Enrollment Upon receipt of a request to change plans or enrollment you should process. As an extra precaution many COBRA plan administrators mail COBRA notices with the United States Postal Service USPS Proof-of-Mailing certificate. After that the plan administrator has 14 days to send you a notice in the mail with information about your coverage where you should send your paperwork.
COBRA beneficiaries generally are eligible for group coverage during a maximum of 18 months for qualifying events due to employment termination or reduction of hours of work. Your cost can be up to 102 of the total cost of the premium with the extra 2 labeled an administrative fee. The law sets down a notice period within which the employer or.
Model Notice in Connection with Extended Election Period. COBRA continuation coverage is often more expensive than the amount that active employees are required to pay for group health coverage since the employer usually pays part of the cost of employees coverage and all of that cost can be charged to individuals receiving continuation. You might be wondering what a qualified event is.
What is COBRA continuation coverage. If you become eligible for other group health coverage such as coverage from a new job or Medicare coverage youre no longer eligible for the COBRA subsidy. MS Word PDF.
COBRA not unlike many employment laws provides grace periods that favor the former employee.
 Cobra Insurance Letter Template Seven Things You Probably Didn T Know About Cobra I Letter Templates Simple Cover Letter Template Cover Letter Template Free
Cobra Insurance Letter Template Seven Things You Probably Didn T Know About Cobra I Letter Templates Simple Cover Letter Template Cover Letter Template Free
 S A M P L E C O B R A L E T T E R T O E M P L O Y E E Zonealarm Results
S A M P L E C O B R A L E T T E R T O E M P L O Y E E Zonealarm Results
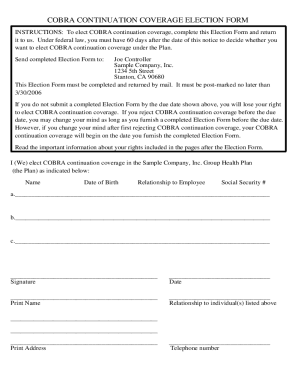
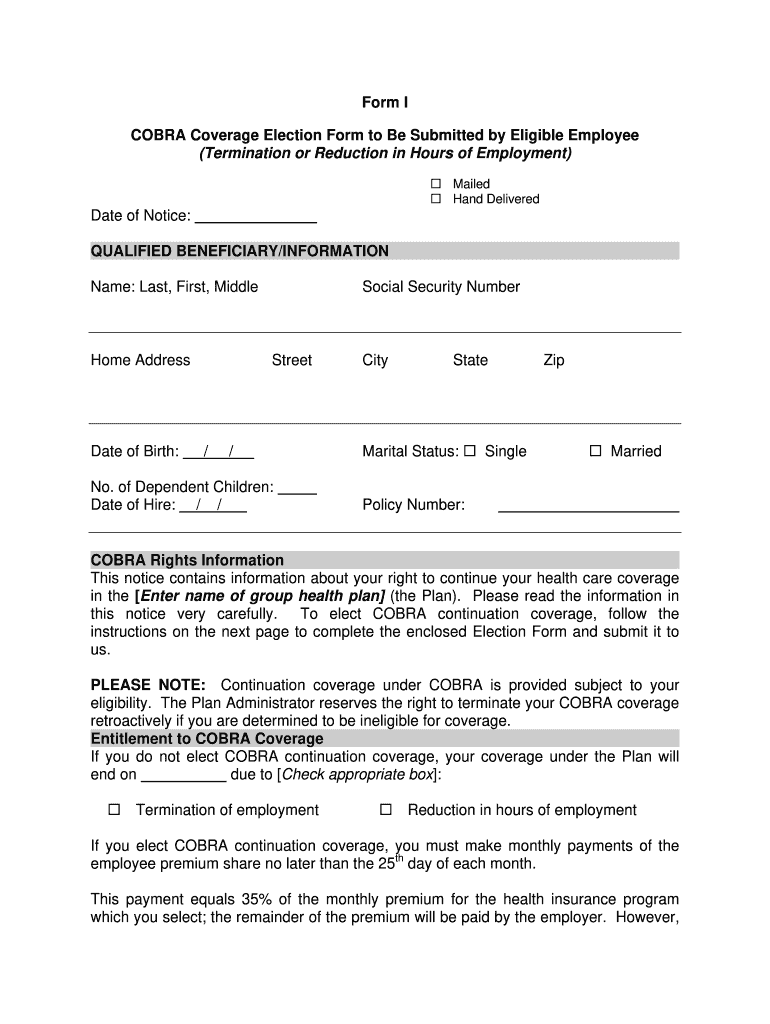
 Blank Cobra Election Forms Fill Out And Sign Printable Pdf Template Signnow
Blank Cobra Election Forms Fill Out And Sign Printable Pdf Template Signnow
Cobra How To Log Into Your Member Portal And Make Your Election 24hourflex
 2013 2021 Cobra Medical Coverage Continuation Form Fill Online Printable Fillable Blank Pdffiller
2013 2021 Cobra Medical Coverage Continuation Form Fill Online Printable Fillable Blank Pdffiller
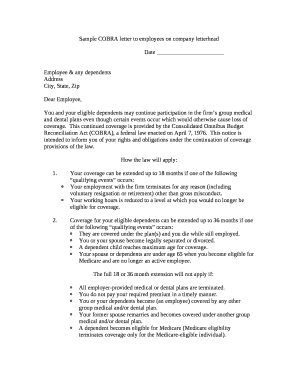 S A M P L E C O B R A L E T T E R T O E M P L O Y E E Zonealarm Results
S A M P L E C O B R A L E T T E R T O E M P L O Y E E Zonealarm Results
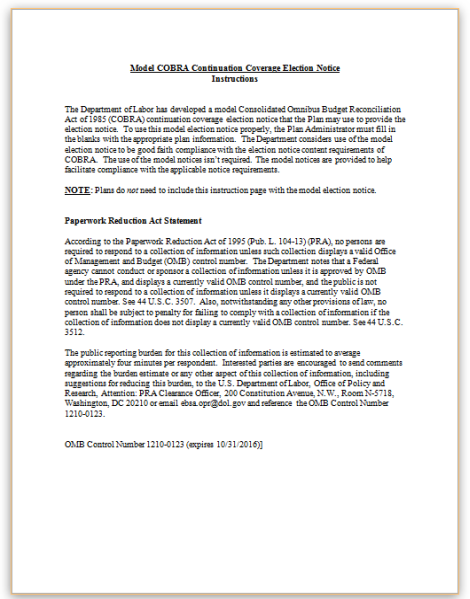
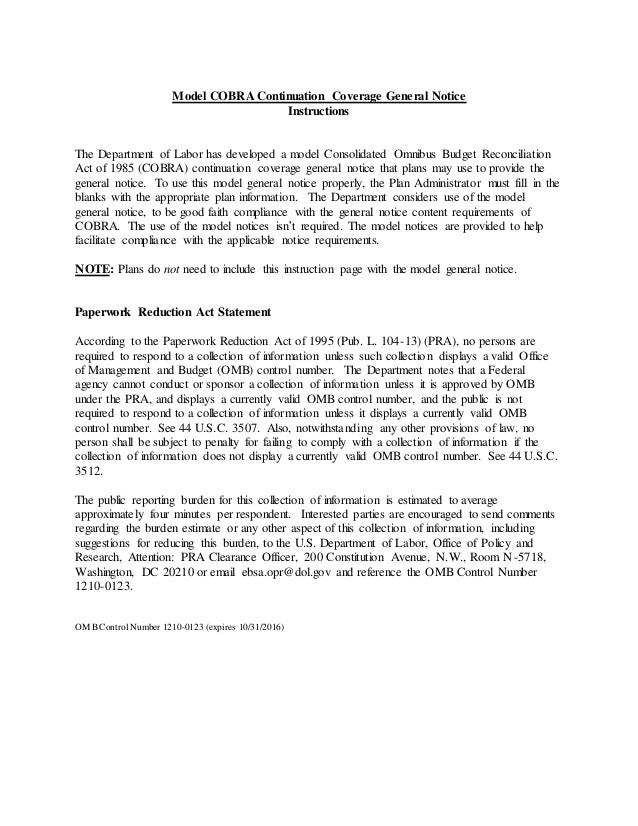
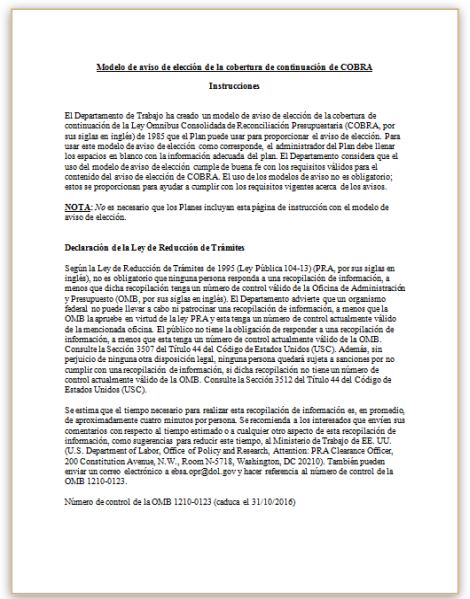
 Model Cobra Continuation Coverage General Notice
Model Cobra Continuation Coverage General Notice
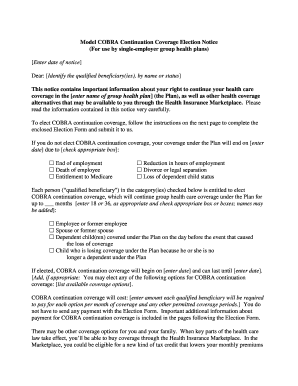
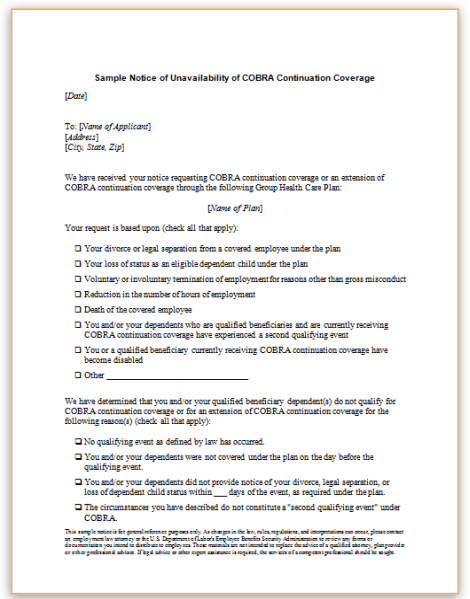
 Cobra Continuation Coverage Election Notice Template Download From Human Resources Policies And Procedures
Cobra Continuation Coverage Election Notice Template Download From Human Resources Policies And Procedures
 Cobra Letter To Employee 2020 Template Fill Online Printable Fillable Blank Pdffiller
Cobra Letter To Employee 2020 Template Fill Online Printable Fillable Blank Pdffiller
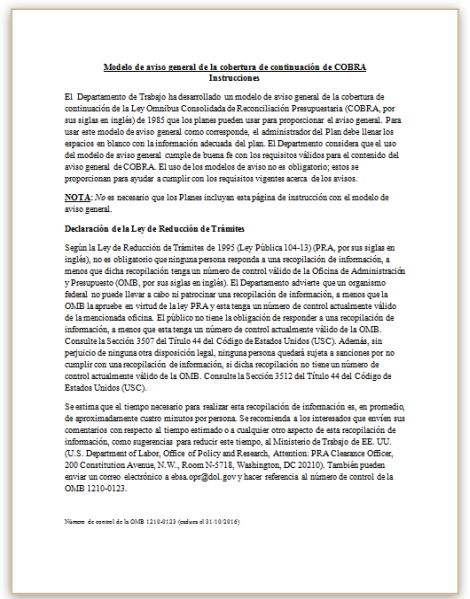
 Model Cobra Continuation Coverage General Notice
Model Cobra Continuation Coverage General Notice

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.