Documented diagnosis of Binge Eating disorder BED AND 2. Drugs Requiring Prior Authorization The listed GCNS may not be an indication of TX Medicaid Formulary coverage.
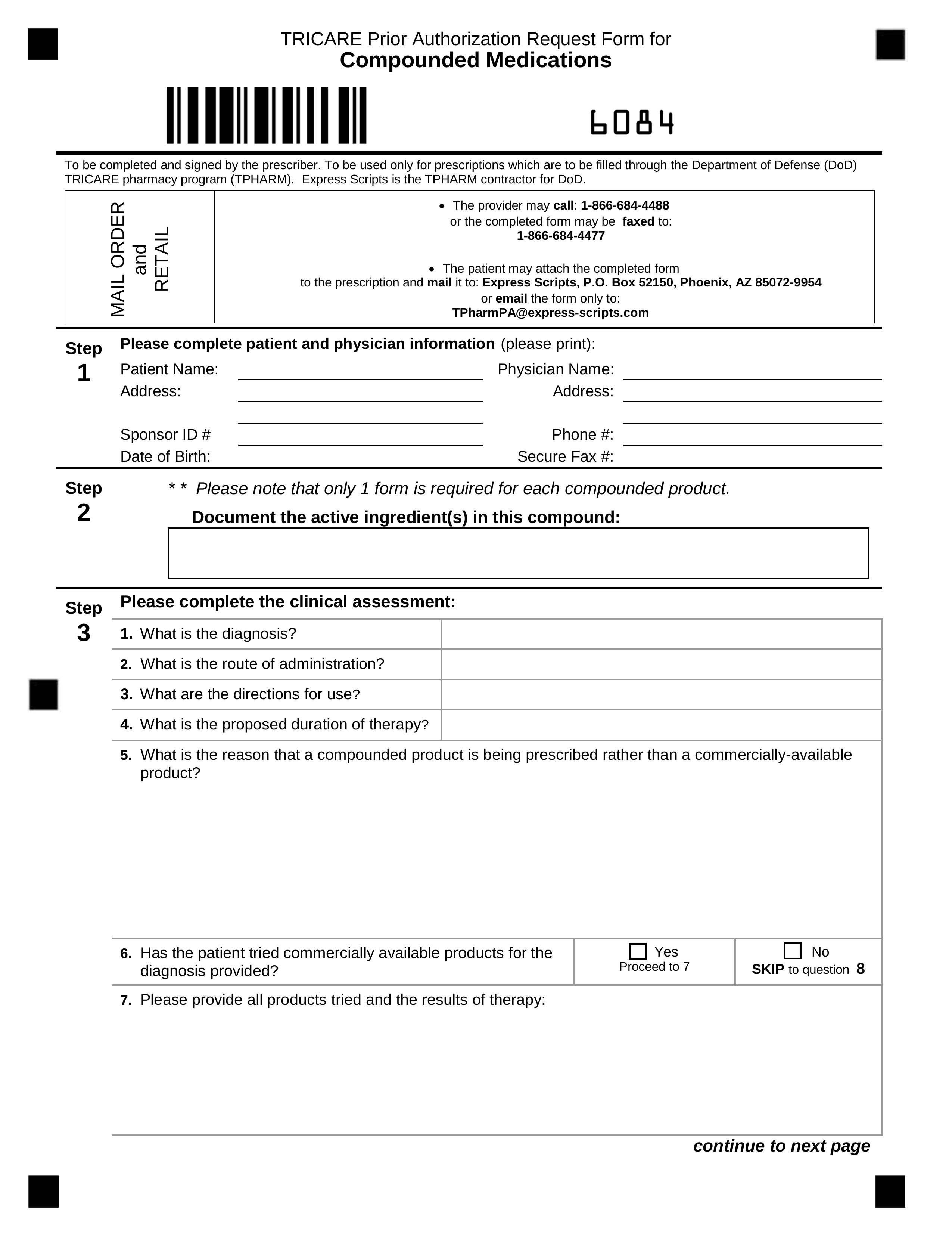 Free Tricare Prior Rx Authorization Form Pdf Eforms
Free Tricare Prior Rx Authorization Form Pdf Eforms
This form applies to Paramount Commercial Select Members Only.
Vyvanse prior authorization. You may need prior authorization for your prescription if it. Box 52080 MC 139 Phoenix AZ 85072-2080 Attn. Attach any additional documentation that is.
Prior authorization for medical necessity. Completereview information sign and date. Fax - 1-855-476-4158 All requests for Vyvanse to Treat Binge Eating Disorder require a Prior Authorization and will be screened for medical necessity and appropriateness using the criteria listed below.
Ask your doctor to choose one of the generic or brand formulary options listed below. Prior Authorization Request Form Caterpillar Prescription Drug Benefit Phone. Prior authorization PA is required for Vyvanse for the treatment of Binge Eating Disorder BED.
Member Information required Provider Information required Member Name. If you continue using one of these drugs without prior approval you may be required to pay the full cost. Attached is a Prior Authorization request form.
Make them prove that your insurance clearly rejected the prior authorization for any reason you just need this paperwork. CNS Stimulants Prior Authorization Request Form Page 1 of 2 DO NOT COPY FOR FUTURE USE. If you are unable to use electronic prior authorization you can call us at 1 800 882-4462 to submit a prior authorization request.
Vyvanse lisdexamphetamine Vyvanse lisdexamphetamine may be covered for Binge Eating Disorder BED if ALL of the following criteria are met and a PA request to Tufts Health Plan using the Universal Pharmacy Medical Review Request Form is submitted. IF THIS IS AN URGENT REQUEST Please Call UPMC Health Plan Pharmacy Services. Medically necessary To be medically necessary means it is appropriate reasonable and adequate for your condition.
Once you receive this paperwork call the company that makes Vyvanse Shire they have a program for people whose insurances dont cover their prescription any longer its called the Shire. Fax signed forms to CVSCaremark at 1-888-836-0730. Prior Authorization Approval Criteria.
Fax completed prior authorization request form to 877-309-8077 or submit Electronic Prior Authorization through CoverMyMeds or SureScripts. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED. We use it to make sure your prescription drug is.
Prior authorization is a restriction put in place by insurance companies so they can decide whether or not they will pay for certain medicines. The Member is at least 18 years of age. You may contact Paramount by phone at 1-419-887-2520 with questions regarding the Prior Authorization process.
PLEASE TYPE OR PRINT NEATLY. Prior to requesting PA Prior to requesting PA the prescriber must review the patients use of controlled substances on the Iowa Prescription Monitoring Program PMP. Used to work behind a pharmacy- also have a family member on Vyvanse here is the advice I can give you.
Drugs Requiring Prior Authorization Label Name GCN VYVANSE 10MG CAPSULE 37674 VYVANSE 10MG CHEWABLE TABLET 42969 VYVANSE 20MG CAPSULE 99366. Please fax signed forms to Paramount at 1-844-256-2025. Please fill out all applicable sections completely and legibly.
When conditions are met we will authorize the. When conditions are met we will authorize the coverage of Vyvanse. Completereview information sign and date.
Vyvanse lisdexamfetamine dimesylate Generic name. 08222018 CAT0279 Page 1 of 2 Instructions. Service Benefit Plan Prior Approval PO.
Fax signed forms to Paramount Advantage at 1-844-256-2025. Eligible patients had to demonstrate treatment response as defined by CGI-S VYVANSE. It doesnt affect cash payment for prescriptions and its only required on those prescriptions when billed through insurance so if youre uninsured or if you decide to pay in cash you wont need to worry about getting prior authorization.
Magellan Rx Management Commercial Clients. UPMC HEALTH PLAN PHARMACY SERVICES PHONE 800-396-4139 FAX 412-454-7722. Incomplete responses may delay this request.
Prior Authorization Criteria Form This form applies to Paramount Advantage Members Only Vyvanse Completereview information sign and date. Please contact Paramount Advantage at 1-419-887-2520 with questions regarding the Prior Authorization process. Prior Authorization Form Amphetamines This fax machine is located in a secure location as required by HIPAA regulations.
For your convenience there are 3 ways to complete a Prior Authorization request. Otherwise please return completed form to. 800-424-7640 2017 2018 Magellan Health Inc.
Have your pharmacy print out the rejection from the insurance company. Subjects were treated with open-label VYVANSE for at least 26 weeks prior to being assessed for entry into the randomized withdrawal period. Please contact CVSCaremark at 1-800-294-5979 with questions regarding the prior authorization process.
Prior Authorization Criteria Form. Vyvanse FEP CSU_MD Fax Form Revised 10182019 Send completed form to. Prior Authorization Prior authorization is a routine process.


.png)