Your health care providers need your BIC to provide services and to bill Medi-Cal. The EBT system is used in California for the delivery redemption and reconciliation of issued public assistance benefits such as CalFresh CalWORKs and other food and cash aid benefits.
Https Www Hpsm Org Docs Default Source Member Manuals Medi Cal Guide For New Members English Pdf Sfvrsn 78d3d4d5 26
Your choices will depend on the county you live in.
State of california benefits identification card website. You also can visit the office in person. Where Can I Use My EBT Card. If you are issued a new card your old card will no longer be valid.
Home Unlabelled State Of California Benefits Identification Card Lost. If your BIC is stolen you must tell your local police and your county social services office. Typically you will receive your Benefits Identification Card BIC immediately.
With luck however you can do an search for the name of your county and the name of your state. Actual card size 3-18x 2-38. Guide To Medi Cal In Santa Clara County.
Beneficiaries of Medi-Cal will have to report any changes to their income family composition other health coverage property etc within 10 days of such change. California The Official Army Benefits Website. If you did not receive your BIC or it is lost or stolen you may ask for a BIC from your county social services office.
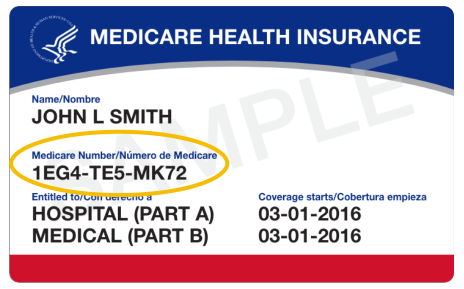
From employee pensions managed by the California Public Employees Retirement System CalPERS to health dental and vision plans state employment offers you many benefits. A BIC looks like this. The 14 numbers and letters on your card identify you.
Effective September 12 2016 a new BIC card design will be implemented. Call your caseworker or your local California Health and Human Services Agency office as soon as you realize your Medi-Cal card is missing. Under the guidance of the California Department of Health Care Services the Medi-Cal fee-for-service program aims to provide health care services to about 13 million Medi-Cal beneficiaries.
Tuesday January 26 2016. Call or visit your local county social services office and ask for a Medi-Cal application. You may also phone the California Department of Health Services to obtain information Medi-Cal.
Medi-Cal mails plastic Benefits Identification Cards BICs to all beneficiaries. If you need more information about recovery or resources visit the following resources. State Of California Benefits Identification Card Lost.
Medi Cal Cards Getting A Facelift California Healthline. The Department of Health Care Services DHCS issues a plastic Benefits Identification Card BIC to each Medi-Cal recipient for identification purposes. If some time has passed and you have not received your BIC in the mail or a letter from DHCS requesting more information you can check your Medi-Cal status by contacting your local Social Services.
Once your provide your name address date of birth Social Security number and other identity-confirming information the representative will disable the lost card and issue a new. You should give as much information about the theft as possible. You have now received or will shortly receive a plastic Benefits Identification Card BIC.
Visit the Medi-Cal website. California has been hit with devastating wildfires and other natural disasters in both the northern and southern parts of the state. This website provides important information for all.
To see the plans available in your county visit the Medi-Cal Managed Care Health Plan Directory. If you do not choose a health plan within 30 days Medi-Cal will choose a plan for you. The California Department of Health Care Services will mail you a Benefits Identification Card BIC if you have been approved for Medi-Cal health insurance.
The BIC is issued by Electronic Data Systems EDS to. TTY users can call. The Savings Plus Program provides additional opportunities to save for.
Recipients of public assistance in California access their issued benefits with the Golden State Advantage EBT card. When you qualify for Medi-Cal you will receive a packet in the mail with health plans you can choose from. All MC clients including Public Assistance PA and Other PA clients ie.
Once there ask for the website address. The Medi-Cal fee-for-service program adjudicates both Medi-Cal and associated health care program claims. This BIC is used to verify your eligibility for Medi-Cal benefits allowing your Medi-Cal providers to bill for your medical andor dental care.
Once you have the site do a. The Benefits Identification Card The Benefits Identification Card BIC is a permanent plastic card that is tied to the clients Medi-Cal Eligibility Data System MEDS record. White card with blue letters on front black letters on back.
Any discrepancies or differences created in the translation are not binding and have no legal. EBT accessible in California the other 49 states the District of Columbia Puerto Rico the Virgin Islands and Guam. The web pages currently in English on the EDD website are the official and accurate source for the program information and services the EDD provides.
The new card design featuring the California poppy will be provided to newly eligible recipients and.