From treating flu and fevers to caring for migraines and allergies you can chat with a doctor 247. When you need care anytime day or night Virtual Visits can be a convenient option.
 Heritage Group Sutter Health Invest 23 6m In Mdlive Mobihealthnews
Heritage Group Sutter Health Invest 23 6m In Mdlive Mobihealthnews
Cost-sharing does apply but will be waived for COVID-19 diagnoses.

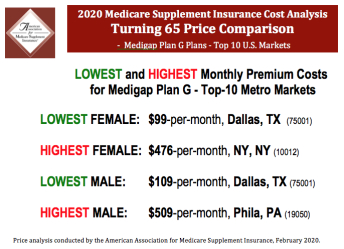
Does mdlive accept medicare. Learn more about Medicare coverage. They have locally-based agents to help assist you with unbiased Medicare plan comparisons and enrollments. The MultiCare Medicare Hotline is serviced by Fletcher Financial Group an independent insurance agency specializing in Medicare.
MDLIVE does not prescribe DEA-controlled substances and may not prescribe non-therapeutic drugs and certain other drugs which may be harmful because of their potential for. Use your mobile device 1 tablet or computer. MDLive works with most major insurance companies including.
After offering the service to a few Medicare Advantage members in Arizona last year Humana is expanding a collaboration with MDLive to make telemedicine services available to Medicare beneficiaries in select counties in Georgia and South Carolina. Even if you go to one that doesnt you have the right to receive care. Can I use MDLive if I dont have health insurance.
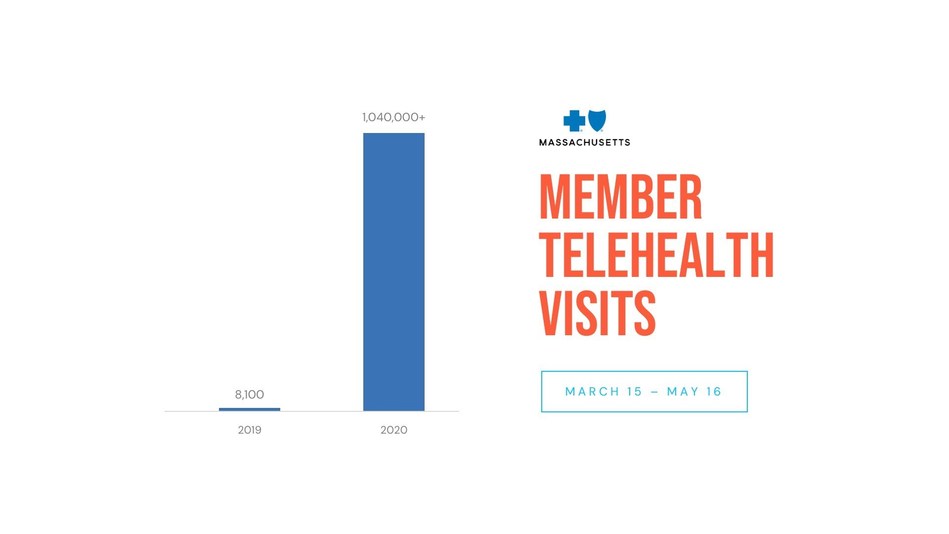
MDLIVEs network is available 247365 including holidays to assist with many non-emergency medical conditions. Telemedicine from MDLIVE is designed to handle non-emergency medical conditions and can often substitute for a doctors office urgent care center or emergency room visit for common conditions like the flu or pink eye. Medicare telehealth services include office visits psychotherapy consultations and certain other medical or health services that are provided by a doctor or other health care provider whos located elsewhere using interactive 2-way real-time audio and video technology.
MDLive is available nationwide. Find affordable quality Medicare insurance plans that meet your needs. Deductibles and cost-shares will then apply.
This temporarily includes audio-only telemedicine visits. A telehealth option to talk to a doctor by phone or video 247. Where is MDLive available.
A telehealth visit allows you to talk with your doctor over the phone instead of visiting a medical facility. If they arent payable by Medicare TRICARE For Life will process as first payer. Mercy Health accepts a variety of health insurance types including commercial Medicare and Medicaid from many local and national health insurance carriers to best serve our communities.
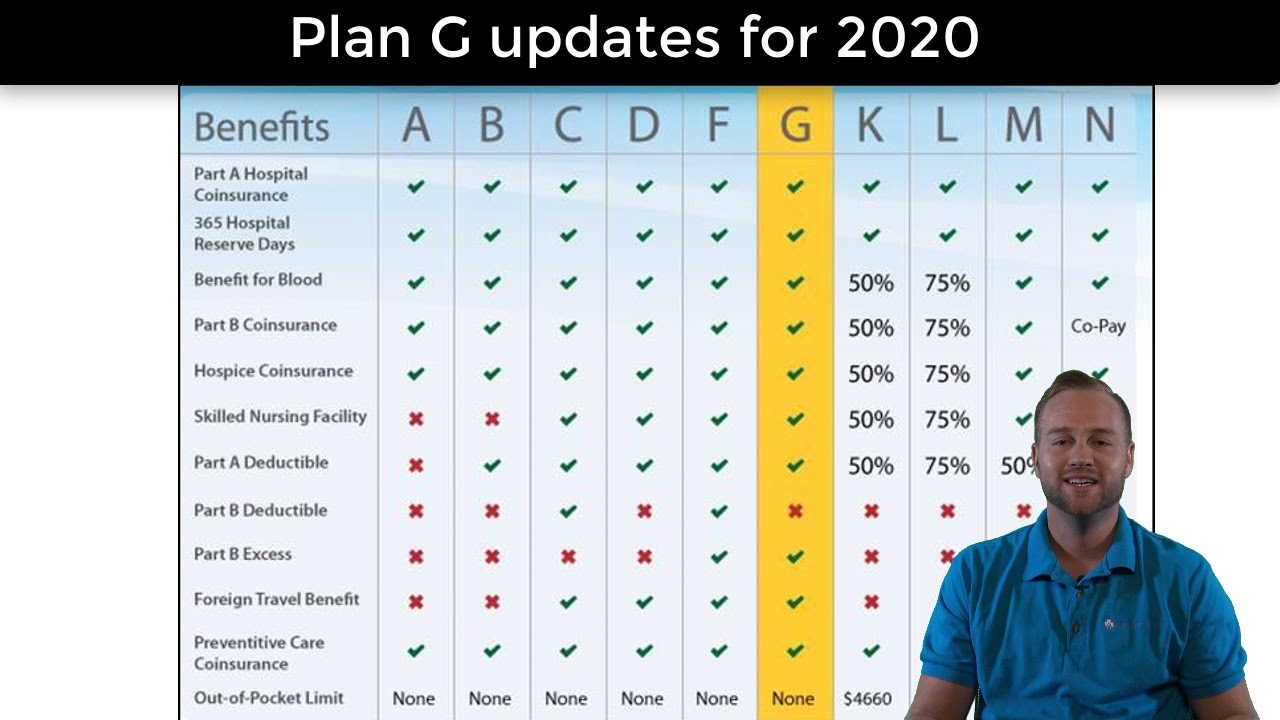
Medicare Part B Medical Insurance covers podiatrist foot doctor foot exams or treatment if you have diabetes-related nerve damage or need Medically necessary treatment for foot injuries or diseases like hammer toe bunion deformities and heel spurs. Medicare Advantage members also have the option of using MDLIVE which is available all year as a filed benefit with zero-dollar cost-sharing. Does MDLive accept insurance.
The Medicare Insurance Helpline is provided to MultiCare patients at no cost and with no obligation. Review the links below for information relevant to your coverage. Anzeige Find your best rate from over 4700 Medicare plans nationwide.
Find affordable quality Medicare insurance plans that meet your needs. Medicare will cover telehealth visits with doctors nurse practitioners clinical. Most urgent care centers do accept Medicare.
Insurance types accepted at Mayo Clinic. Anzeige Find your best rate from over 4700 Medicare plans nationwide. Our doctors can diagnose treat and even prescribe medication when appropriate providing care whether youre a home at the office or on the go.
MDLIVE does not replace the primary care physician is not an insurance product and may not be able to substitute for traditional in-person care in every case or for every condition. In this case the urgent care center will. Can members do wellness visits through telemedicine.
Humana to offer MDLive telemedicine to some Medicare Advantage members. You can sign up for the platform and pay for telehealth visits out of pocket. To check if our hospital is contracted with your insurance choose the hospital location you plan to.
If you use TRICARE For Life Medicare should cover telemedicine visits when the service and provider are payable by Medicare. Mayo Clinic has established arrangements with several different types of health care insurers.






:max_bytes(150000):strip_icc()/medicare-part-d-costs-4589863_FINAL-a334073127ad461fbd5457a7d74d1e6c.png)



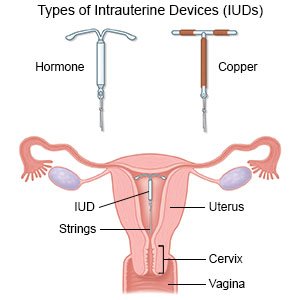
/iud-strings-missing-906756_color2-5b92cc2cc9e77c008290970c.png)