You may find these on. It doesnt affect cash payment for prescriptions and its only required on those prescriptions when billed through insurance so if youre uninsured or if you decide to pay in cash you wont need to worry about getting prior.
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
This is extremely important to know especially for people being treated for cancer.

How does prior authorization work. PA is a technique for minimizing costs. Like sands through the hourglass so are the days of prior authorization. The toll of prior authorization is rising they said.
How does the prior authorization process work. Prior authorization is a restriction put in place by insurance companies so they can decide whether or not they will pay for certain medicines. These figures come from the responses to a 27-question web-based AMA survey administered to 1000 American physicians who provide at least 20 hours of patient care per week.
Prior authorization and pre-claim review are similar but differ in the timing of the review and when services may begin. And thats why we have programs like prior authorization. Health insurance companies use prior authorization to verify that a certain drug procedure or treatment is medically necessary before it is done or prescribed.
Your insurance provider. Medications that have lower-cost equally effective alternatives available. How Do I Get Prior Authorization for a Medication.
If its determined that your plan doesnt cover the drug you were prescribed you can ask your doctor. Your insurance company will contact you with the results to let you know if your drug coverage has been approved or denied or if they need more information. If a PA is needed locate the process for submitting and obtain any required prior authorization forms.
Certain medications may need approval from your health insurance carrier before theyre covered. When your doctor prescribes a medication you trust its the right one for you. Prior authorizations for prescription drugs are handled by your doctors office and your health insurance company.
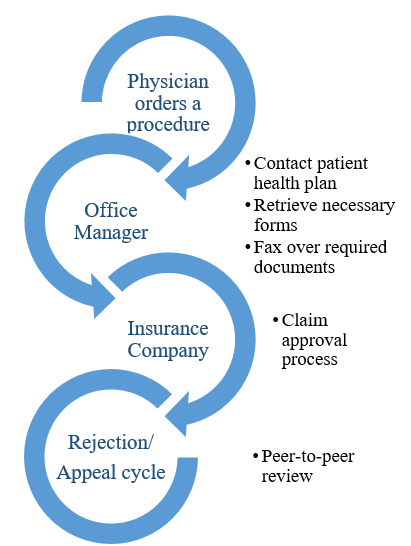
It is the process of getting approval from your health insurance company not your doctor to obtain a prescription or treatment as demonstrated below. Medications that may be unsafe when combined with other medications. How to Get Prior Authorization after the fact.
Check your plans policy documents and formulary to see if any of your treatments require a PA. Nearly 90 percent of the physicians. Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance.
The physician will contact the insurance company and submit a formal authorization request. Health insurance companies use the prior authorization or pre-approval process to verify that a certain drug procedure or service is medically necessary BEFORE it is done or the prescription is filled. Prior authorization PA is a requirement that your physician obtain approval from your health insurance plan to prescribe a specific medication for you.
I understand that pre-authorizations for more than the amount of the room are fairly common for hotels to be sure the guest has sufficient credit to cover additional expenses such as room damage and optional amenities but I have read that generally on check-out the final amount is charged in ADDITION to the pre-authorization and then the pre-authorization drops from the. Medications that are often used for cosmetic purposes. Prior authorization ensures that you get the prescription drug that is right for you and that is covered by your benefit.
If it is discovered that prior authorization is required when. Thats not always the case. When we review certain drugs before your plan covers them it helps make sure youre getting the right medication for.
Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. Using our career map a prior authorization specialist can determine their career goals through the career progression. For example they could start out with a role such as pharmacist progress to a title such as manager and then eventually end up with the title office manager.
Under prior authorization the provider or supplier submits the prior authorization request and receives the decision prior to rendering services.
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 Webinar Recording Implementing Centralized Electronic Prior Authorization Youtube
Webinar Recording Implementing Centralized Electronic Prior Authorization Youtube
 Prior Authorization Understand It And Simplify It Patients Rising
Prior Authorization Understand It And Simplify It Patients Rising
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 Charm Ehr Electronic Prior Authorization Epa
Charm Ehr Electronic Prior Authorization Epa
 Prior Authorization Automation Case Study Webinar With Cleveland Clinic And Priorauthnow Youtube
Prior Authorization Automation Case Study Webinar With Cleveland Clinic And Priorauthnow Youtube
Real Time Automated Prior Authorization Via Edi 278
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare

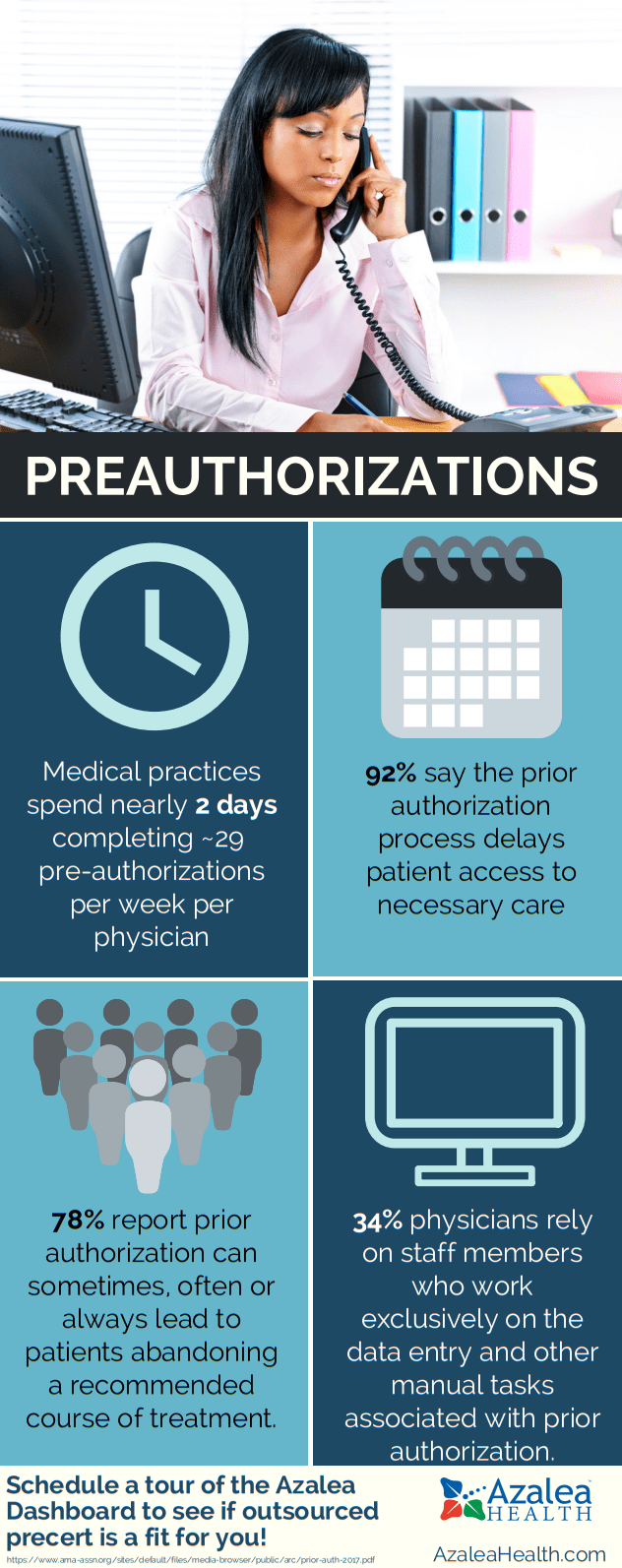 Prior Authorizations Azalea Health
Prior Authorizations Azalea Health
 Electronic Prior Authorization For Faster Approvals Surescripts
Electronic Prior Authorization For Faster Approvals Surescripts
 Pre Authorization Best Practices Webinar
Pre Authorization Best Practices Webinar
 Pre Authorization And Pre Certification
Pre Authorization And Pre Certification
 Prior Authorization The Filibuster Of Healthcare Aans Neurosurgeon
Prior Authorization The Filibuster Of Healthcare Aans Neurosurgeon

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.