Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association. The Blue Cross name and symbol are registered marks of the Blue Cross Association.
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Electronically submit authorization requests for behavioral health medical and surgical services.

Blue cross authorization. Independent licensees of the Blue Cross Association. For more information on criteria for special authorization please click here PDF. If the request for prior authorization isnt approved your insurer will let you and your doctor know.
Your doctor will submit a prior authorization request before ordering a test or medication. Requests for the following services can be made by fax or mail. Authorization is required for the following services.
This page provides Blue Cross Blue Shield of Michigans authorization requirements including information that applies to. 521 Zeilen Requests for special authorization are considered for adults as adjunct to diet and. Requests will be confidentially reviewed according to payment criteria developed by Blue Cross in consultation with.
Cardiology services - Medicare Plus Blue SM. In addition we recommend preauthorization for all elective inpatient admissions some procedures that may be considered cosmetic and before services are performed outside the local participating provider network. Medicare Plus Blue SM PPO.
Drug Special Authorization Request Form. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. ANTHEM is a registered trademark of Anthem Insurance Companies Inc.
This includes cardiac implantable devices and services for dates of service on or after Jan. If that happens you and your doctor may choose another treatment option or offer more info so the request can be reviewed again. The Blue Cross Blue Shield Association is an association of 35 independent locally operated Blue Cross andor Blue Shield companies.
If we determine that the services are medically necessary we send an approvalor authorizationin writing to the member primary care provider PCP the treating physician and the facility if applicable to let them know that we have approved the services. They can be printed then completed and signed by hand or they can be filled in on-line printed and then signed before sending to Alberta Blue Cross. Blue Cross and BCN Prior Authorization and Step Therapy Guidelines Site of Care Program.
Preauthorization is required or recommended based on the plan for a number of services and drugs as noted in our policies. Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Authorization Manager available 247 provides an alternative to Online Services allowing you to. You will be provided the prior authorization requirement or directed to the potential medical policy for additional clinical criteria. If that happens you and your doctor may choose another treatment option or offer more info so the request can be reviewed again.
When a request for service is not approved we notify the PCP and the member. Prior Authorization is a pre-approval process to determine if certain prescription drugs will be reimbursed under a members benefit plan. Submit a Blue Shield Promise medical or pharmacy authorization To submit a medical or pharmacy authorization visit the Provider forms page and click Authorization Request request forms.
Information please contact an Alberta Blue Cross privacy matters representative toll-free at 1-855-498-7302 or write to Privacy Matters Alberta Blue Cross 10009 108 Street Edmonton AB- T5J 3C5. Click the special notice at the top of the Provider Secured Services home page. Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests.
Your doctor will submit a prior authorization request before ordering a test or medication. Anthem Blue Cross is the trade name of Blue Cross of California and Anthem Blue Cross Partnership Plan is the trade name of Blue Cross of California Partnership Plan Inc. This program redirects members receiving select injectable or infusible drugs in the outpatient hospital setting to a lower cost alternate site of care such as the physicians office or members.
O Outpatient interventional pai n management o Inpatient and outpatient lumbar spina l fusion surgery o Outpatient radiation therapy oncology for Medicare Plus Blue and Blue Cross PPO o Outpatient physical and occupational therapy services and inpatient post -acute care. AIM-Managed Procedures for Blue Cross. Blue Cross commercial PPO only.
Complete the form and fax the request to the fax number listed in the upper right-hand corner of the form. If the request for prior authorization isnt approved your insurer will let you and your doctor know. The Blue Cross symbol and name are registered marks of the Canadian Association of Blue Cross Plans an association of independent Blue Cross plans.
Submit a prior authorization Reviewed by BlueCross BlueShield. Taking Action to Address Racial Health Disparities Learn how Blue Cross and Blue Shield companies are addressing our nations crisis in racial health disparities at our new Health Equity website. Providers must obtain authorization from AIM Specialty Health for the following services.
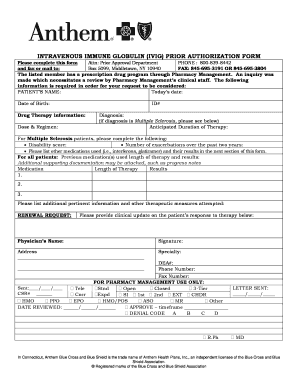
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Https Bluecrossnc Com Sites Default Files Document Attachment Common Pdfs Hmo Ppo General Quantity Limitations Fax Request Form Pdf
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
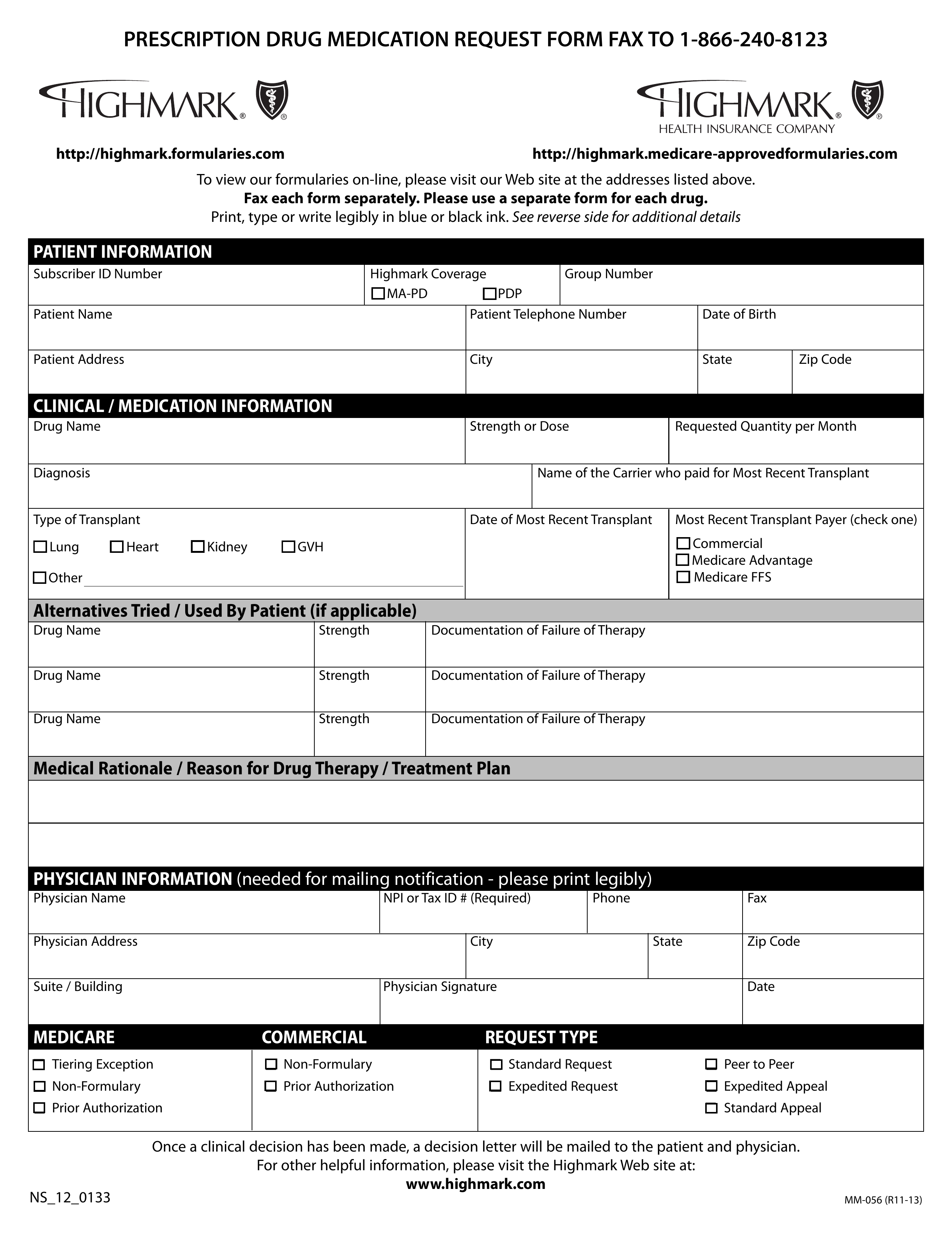 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
 Alberta Blue Cross Celecoxib Special Authorization Request Form Juno Emr Support Portal
Alberta Blue Cross Celecoxib Special Authorization Request Form Juno Emr Support Portal
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
Https Providers Bcbsal Org Portal Documents 10226 301829 General Prescription Drug Coverage Authorization Request Form A9b9b8bf 922b 469a B21f E396da68c634 Version 1 5
Https Www Blueshieldca Com Bsca Bsc Public Common Portalcomponents Provider Streamdocumentservlet Filename Prv Fep Medical Injectable Drug Pdf
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
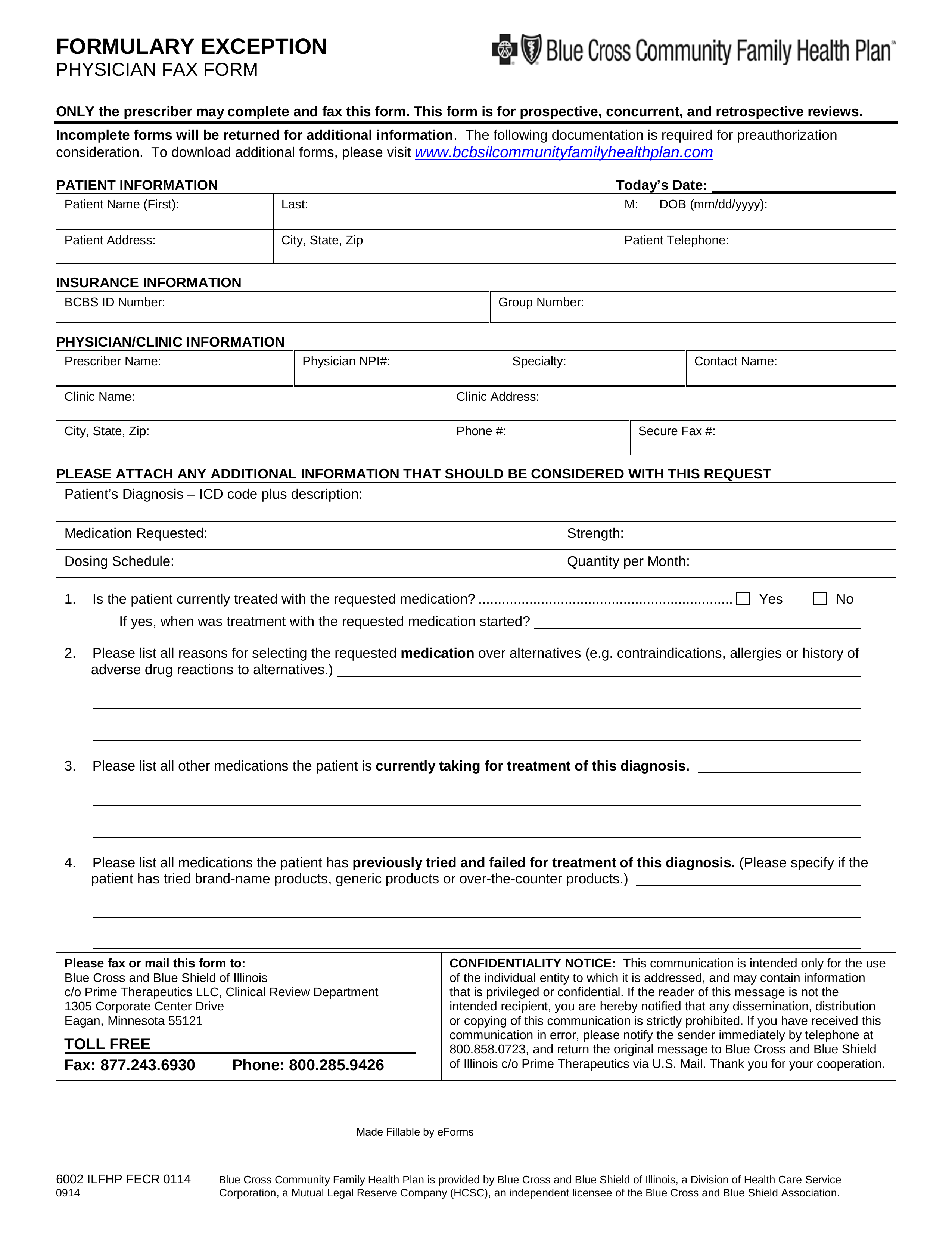
 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
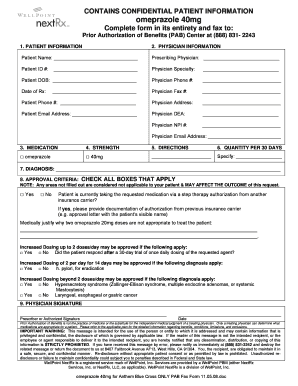
 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.