Blue Cross Blue Shield breast reduction will cover your breast reduction in many cases but only if you fulfill their criteria. Disturbances related to the large breast size.
 Signs You Need A Breast Reduction Plastic Surgery Advice In Baton Rouge Weiler Plastic Surgery
Signs You Need A Breast Reduction Plastic Surgery Advice In Baton Rouge Weiler Plastic Surgery
Decompression of the Intervertebral Disc Using Laser Energy Laser Discectomy or Radiofrequency Coblation Nucleoplasty Denosumab Prolia XGeva Dental Inpatient and Outpatient Services.
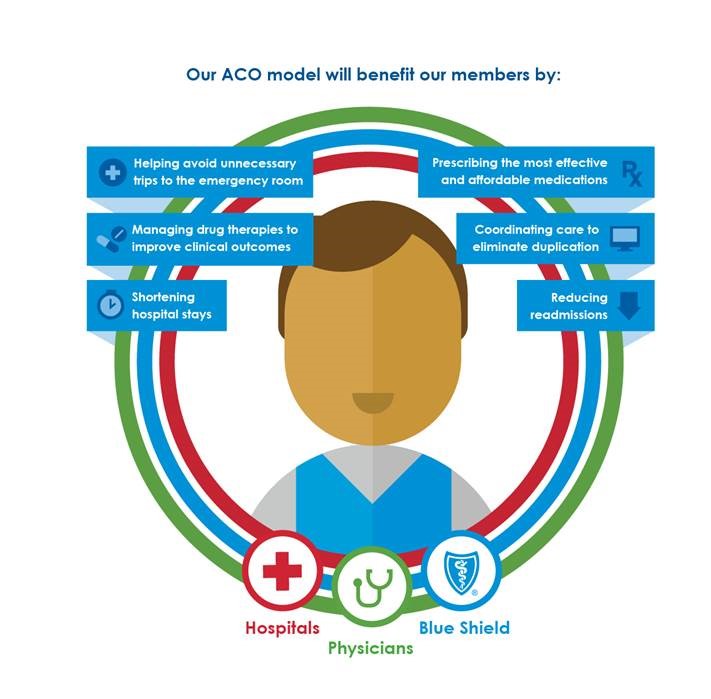
Blue shield breast reduction coverage. Breast Reduction Reduction Mammaplasty for Systematic Breast Hypertrophy or Hypermastia No Photos Needed Reduction Mammaplasty for symptomatic breast hypertrophy or hypermastia may be considered allowable for coverage when there is supporting medical documentation and ALL of the medical criteria are met. It is considered reconstructive in attempts to obtain insurance coverage for the surgery but it is also considered cosmetic in that patients expect meticulous aesthetic expertise in their surgery and results. Does BCBSIL Cover Breast Reduction Surgery.
None Reduction Mammaplasty for Breast-Related Symptoms Description Macromastia or gigantomastia is a condition that describes breast hyperplasia or hypertrophy. Each insurance company such as Blue Cross Blue Shield has its own standards on what qualifies a patient for insurance coverage of a breast reduction. Read Your Insurance Coverage Materials Previous.
March 2012 Related Policies. Reconstructive procedures that may be considered cosmetic. Supply is medically necessary does not constitute a representation or warranty that the Blue Cross and Blue Shield Service Benefit Plan covers or pays for this service or supply for a particular member.
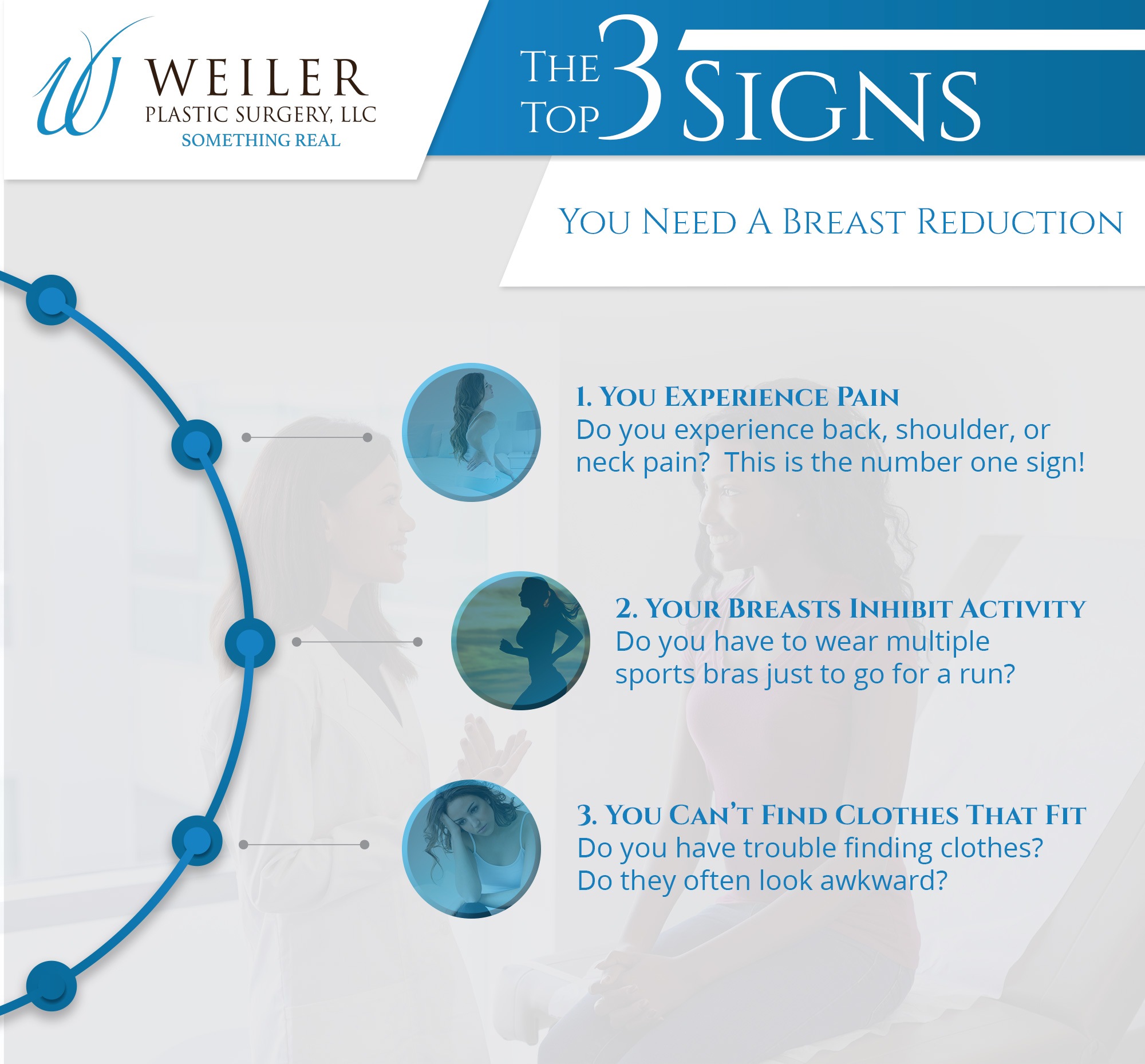
Does Blue Cross Blue Shield Cover Breast Reduction. If you have the right symptoms but the breasts arent large enough they may not approve the surgery. The criteria are the symptoms like back and neck pain rashes under the breasts and large breasts.
Blepharoplastycanthopexycanthoplasty excision of excessive skin due to weight loss rhinoplastyrhytidectomy pectus excavatum repair breast reconstructionenlargement breast reductionmammoplasty lipectomy or excess fat removal sclerotherapy or surgery for varicose veins facial reconstruction or repair including. Macromastia may result in clinical. Insurance coverage of breast reduction.
Another proposed method of mammaplasty involves the suction of fatty tissue from the breast liposuction. The presence of symptoms related to your large breast size such as neckbackshoulder pain are important in showing medical necessity which it sounds like you have from your description. The mastectomy need not have been performed while the.
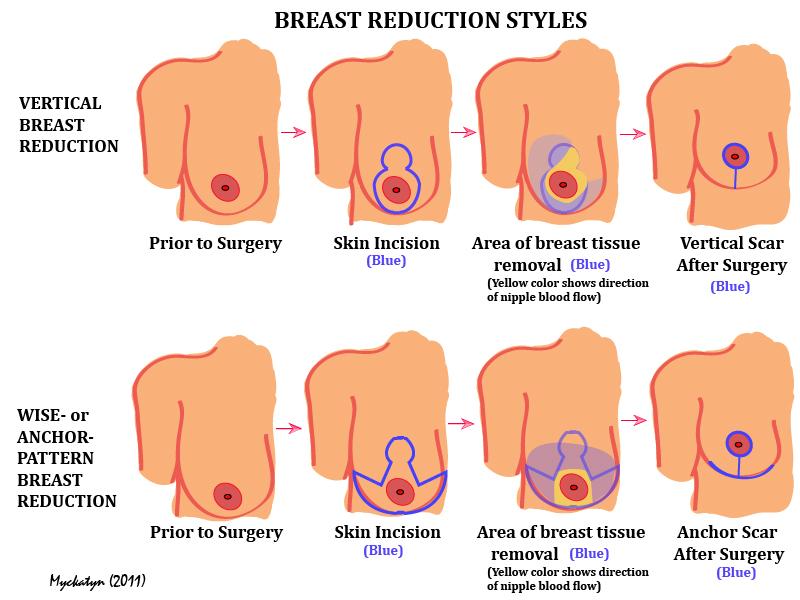
For individuals who have symptomatic macromastia who receive reduction mammaplasty the evidence. July 1 2019 Original Policy Date. Reduction mammaplasty is a surgical procedure designed to remove a variable proportion of breast tissue to address emotional and psychosocial issues andor to relieve the associated clinical symptoms.
Reduction Mammaplasty for Systematic Breast Hypertrophy or Hypermastia Answer. Any major surgical treatment has significant risks. Yes if you meet their list of requirements and receive a pre-authorization.
Read Your Insurance Coverage Materials. Breast reduction surgery is a covered benefit if determined medically necessary by an IPA Physician. BCBSNC will cover Reconstructive Breast Surgery after Mastectomy Surgical Treatment of Gynecomastia Reduction Mammaplasty for Breast Related Symptoms Risk-Reducing Mastectomy and Surgical Management of Breast Implants when it is medically necessary because the criteria shown below have been met.
The procedure is designed to reconstruct the breast with an aesthetically acceptable appearance while reducing the breast mass. Reduction Mammaplasty for Breast-Related Symptoms. In our practice it has become increasingly difficult to obtain insurance coverage for breast reduction surgery.
Breast reconstruction post- mastectomy is also covered. The most common method of breast reduction involves the surgical removal of skin fat and breast tissue. Some insurance companies cover some or all of the costs of breast reduction surgery if surgery is being done to relieve back pain skin problems or other medical problems caused by large or heavy breasts.
Breast reduction may also be covered in females for whom growth is complete 18 years of age or older who have enlarged breasts macromastia when the following criteria have been met. Usually that includes back and neck pain rashes under the breasts and large breasts which are large enough. Wed recommend talking over these requirements with your doctor as they will be more familiar with the pre-auth process.
FEP 70121 Reduction Mammaplasty for Breast-Related Symptoms. Insurance companies have different criteria for coverage of breast reduction surgery including symptoms attributable to the weight of the breasts such as pain and bra grooving and amount of breast tissue expected to be removed at the time of the surgery mass in grams. Having bra strap grooving on your shoulders and.
The Womens Health and Cancer Rights Act of 1998 WHCRA is federal legislation that provides that any individual with insurance coverage who is receiving benefits in connection with a mastectomy covered by their benefit plan whether or not for cancer who elects breast reconstruction must receive coverage for the reconstructive services as provided by WHCRA. Any of the following symptoms for at least 12 months as documented in the patients records. FEP 70121 Reduction Mammaplasty for Breast-Related Symptoms Effective Policy Date.
They typically will not cover breast reduction surgery being done solely to change the appearance of the breasts because it is not considered a medically necessary procedure when done for this reason. You must know that if you have not had large enough breasts they will not approve the surgical operation. Email protected Home Breast Reduction.
Blue Cross Blue Shield generally will cover a breast reduction if you meet their criteria. Next Tweet 2021 - Breast Reduction by Amber McConnell mail.