Please contact your provider representative for assistance. If we approve the request payment is still subject to all general conditions of Anthem Blue Cross and Blue Shield including current member eligibility other insurance and program restrictions.
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
Prior authorization requirements apply to all of the HealthSelect plans except HealthSelect SM Secondary.
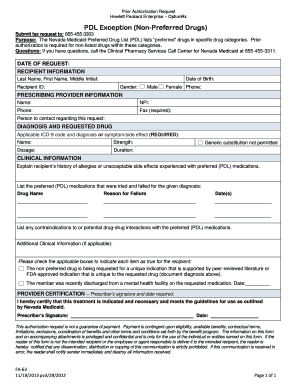
Empire blue cross blue shield prior authorization form. Submit prior authorization requests to AIM. PRIOR AUTHORIZATION REQUEST FORM REQUESTED AGENT. Go to the preapprovals section below for more information.
Does Empire require a prior authorization on the focused test used to diagnose COVID-19. This means your doctor must get approval from us before they can write a prescription for the drug. This form is to be filled out by a member if there is a request to release the members health information to another person or company.
Prior authorization PA form synagis. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. By Phone Call the AIM Contact Center at 1-800-859-5299 Monday through Friday 6 am.
Blue Cross Blue Shield of Massachusetts Health Plan Phone. Anthem has also made available a series of forms. Its called a Preferred Drug List PDL.
In general your network PCP and other network providers are responsible for obtaining prior authorization before they provide these services to you. If you do not obtain prior approval there may be. To help us expedite your authorization.
Medicaid precertification auth request form. Provider Forms Guides. Anthem Blue Cross and Blue Shield in New Hampshire.
All Forms Guides. BCBSTX must approve certain covered health services before you get them. Drugs not listed on the PDL always require preapproval.
There are some covered health services however for which you are responsible for obtaining prior. Certain medical services and treatments need approval before you receive care. Andor Empire HealthChoice Assurance Inc licensees of the Blue Cross and Blue Shield Association an association of independent Blue Cross and Blue Shield plans.
Please complete this form and fax or mail to. Prior authorization form for contraceptives for essential plan. This is called prior approval precertification or preauthorization.
Andor Empire HealthChoice Assurance Inc licensees of the Blue Cross and Blue Shield Association an association of independent Blue Cross and Blue Shield Plans. The following guidelines apply to Anthem Blue Cross and Blue Shield Anthem products issued and delivered by Anthem in New Hampshire. Complete the form and fax the request to the fax number listed in the upper right-hand corner of the form.
At Anthem were committed to providing you with the tools you need to deliver quality care to our members. Prior authorization PA form medical injectables. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
For information on precertification requirements for those members of National. We will notify the provider and the members pharmacy of our decision. 1 2021 in one of the following ways.
We review them to ensure they are medically necessary. When applicable for Jan. Any incomplete sections will result in a delay in processing.
Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. Services provided by Empire HealthChoice HMO Inc. We review requests for prior authorization based on medical necessity only.
Blue Shield Medicare Non-Formulary Exception and Quantity Limit Exception PDF 129 KB Prior AuthorizationCoverage Determination Form PDF 136 KB Prior. May 30 2018 State Federal Medicaid. To 6 pm CT.
The scope of this notice will include both professional and facility requests for Medicaid business. Complete this form in its entirety. Receive a current member handbook and a provider directory.
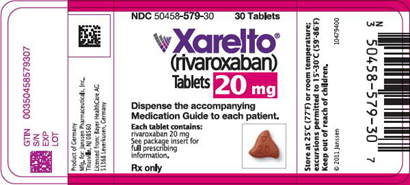
Many of the drugs listed on the PDL do not need preapproval. Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax it to 877 327-8009. Select the Drug List Search tab to access up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug.
Destination Where this form is being submitted to. Does Empire require use of a contracted provider for the COVID-19 lab. Services provided by Empire HealthChoice HMO Inc.
Specialty medications that are reported with not otherwise classified NOC designation codes. No prior authorization is not required for diagnostic services related to COVID-19 testing. This is called a prior authorization.
Online Submit requests via the AIM ProviderPortal 247. Payersmaking this form available on their websites may prepopulate section A Health Plan or Prescription Plan Name. Submit a Blue Shield Promise medical or pharmacy authorization To submit a medical or pharmacy authorization visit the Provider forms page and click Authorization Request request forms.
All programs require prior authorization PA for all covered specialty medications where allowable by state. Empire has a list of preferred drugs chosen for their quality and effectiveness. Receive the necessary information to be an Empire BlueCross BlueShield HealthPlus Empire member in a manner and format they can understand easily.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. On this page you can easily find and download forms and guides with the information you need to support both patients and your staff. Empire BlueCross BlueShield HealthPlus information.