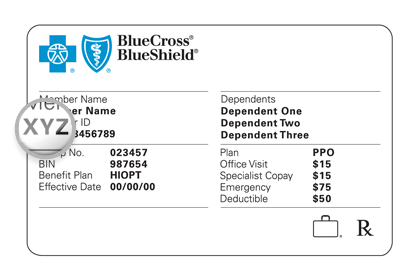
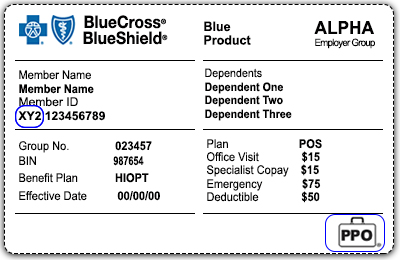
Of the Blue Cross and Blue Shield Association Customer Service. Most Blue Cross and Blue Shield BCBS branded ID cards display a three-character prefix in the first three positions of the members ID number.
Https Www Bluecrossmn Com Sites Default Files Dam 2020 09 P11ga 12956593 Pdf
You either have the Blue Cross and Blue Shield of Vermont Formulary or the National Performance Formulary.

Blue cross blue shield rx bin number. 888-826-8152 VSP - Vision. It will be the same for everyone covered under your Horizon BCBSNJ plan and will remain as your ID number for as long as you are the subscriber of the health plan. The member ID number begins with the letter H.
View your Pharmacy Benefits. The letter will tell you which drug list or formulary your patients plan uses. 2021 Horizon Blue Cross Blue Shield of New Jersey Three Penn Plaza East Newark New Jersey 07105.
If you are a BCBSIL member log in to Blue Access for Members SM BAM SM to check your drug list and learn more about your prescription drug benefits. What is an Rx group. If you suspect fraudHMO 800-482-3787 Mental healthsubstance abuse treatment.
Log in to chat in Blue Access for Members SM Monday Friday 8 am. It means they have medication coverage. Member ID numbers always start with three letters known as the alpha-prefix.
1 Look for the Rx on their member ID card. ID cards for the following products and programs do not have a three-character prefix. 1Ø1-A1 BIN NUMBER Multiple M BINs listed in General Information Section 1Ø2-A2 VERSIONRELEASE NUMBER DØ M 1Ø3-A3 TRANSACTION CODE B1 M 1Ø4-A4 PROCESSOR CONTROL NUMBER Multiple M PCNs listed in General.
If you have any questions about your prescription drug benefits call the number on your member ID card. Generally the numbers after the 3HZN are what doctors and hospitals will need from you. As a Premera-contracted provider you can render services to patients who are national account members of other Blue Cross andor Blue Shield plans and who travel or live in your state.
BIN 610014 Bank Identification Number. However there are some exceptions. If a Blue Cross Blue Shield of Massachusetts member has designated a PCP you can learn their name and telephone number by performing an eligibility inquiry using an electronic technology such as Online Services.
Formulary Drug Lists. You can have certain prescriptions delivered right to your door when you order them through Express Scripts an independent company that administers your pharmacy benefits on behalf of Blue Cross Blue Shield of Massachusetts. Commercial HMO POS.
Applicable ProductsCommercial PPOEPO Exchange POSEPO Applicable Products. If you have any questions about your prescription drug benefits call the number on your member ID card. Determine what prescription drugs are covered under your plan or may require approval before you have them filled.
Be sure to review your benefit materials for details. Claims should be transmitted using Bin Number 012833. This is the number Blue Care Network assigns to you.
Be sure to review your benefit materials for details. Health care providers use it to identify you and your benefts. Arkansas Blue Cross Blue Shield Medi-Pak Rx PDP Ø16895 PDPAR.
800-810-2583 Misuse may result in prosecution. In some cases youll pay less for a 90-day supply of maintenance medications also known as long-term medications than you would for three 30-day supplies at a. If you are a BCBSTX member log in to Blue Access for Members SM BAM SM to check your drug list and learn more about your prescription drug benefits.
The BIN assists pharmacies with submitting prescription medication claims through the Medco on-line system. 800-257-9980 To locate participating providers outside of Michigan. Your 1 Member ID number 2 Rx BIN 3 PCN and 4 Group ID or Rx Group number are the four numbers that uniquely identify you and your Medicare Part D prescription drug plan - and these four numbers are usually found on your Medicare Part D Member ID card and most of you Medicare plan correspondence or printed.
1 2 3 4 5 6 9 8 7 1. Process Control Number PCN for BlueScript Mediscript and BlueCare Rx members is FLBC and the member ID number is the letter H followed by 8 or 10 numeric digits. 2 Look for a capital letter or a capital letternumber combination after the Rx on your patients card.
This is the person who has the coverage it may be you your spouse or your parent. Member ID number Your member ID number is made up of a series of letters and numbers. Blue Blue Member Number BC BS Rx BIN PCN Group Number Member Number BC BS Rx BIN PCN Group Number XJK901000019 XJK901000019 090 590 090 590 _____ _____ _____ _____.
/cdn.vox-cdn.com/uploads/chorus_asset/file/21902481/trump_admin_birth_control_board_1.jpg)